Covid-19 has brought much of the world to a halt this year. However, it is just one of the many infectious diseases without a vaccine that affect millions of people around the world. The development of therapeutics for these infectious diseases has mostly been overlooked by pharmaceutical companies in favor of higher-margin therapies for the developed world. Creating therapeutics for these viral pathogens can take years of clinical and regulatory assessment before they become available to those who need them.
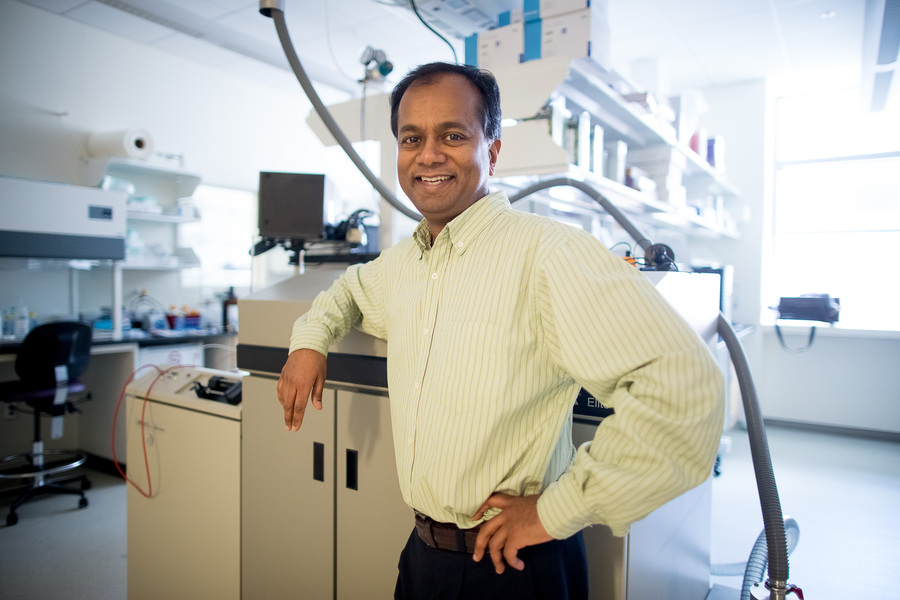
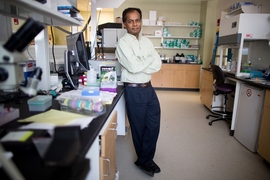
Ram Sasisekharan, the Alfred H. Caspary Professor of Biological Engineering, has been at MIT since 1996 and is a principal investigator of the Antimicrobial Resistance Interdisciplinary Research Group at the Singapore-MIT Alliance for Research and Technology (SMART), MIT’s research enterprise in Singapore. His work seeks to condense the time taken to develop therapeutics down from many years to a matter of months.
Q: How has your work helped to speed up the development of therapeutics for infectious diseases?
A: I have always had a fascination with solving problems. My career progressed as I began looking for solutions that other people hadn’t investigated before. On the way, I took an interest in regulatory science, in terms of how drugs are developed, tested for safety and efficacy, and brought to market.
It is not as easy as simply thinking that you have a vaccine or therapy to conquer a disease and then releasing it to the public. Before you can do so, all the levels of non-clinical and clinical trials have to come together, which is not a fast process. Current drug development models are very linear and can take five to 10 years — and an extraordinary amount of money — before they pan out. A lot of drugs will fail, so we need to take a lot of shots on goal before we can deliver the right therapy and vaccines.
The better we understand a disease, the faster we can move. For example, dengue, Zika, and yellow fever broadly belong to the same family of viruses, which allows us to use what we learn in one of these viruses for the others, to some extent. We found that these viruses bind to carbohydrates (or glycans) on the surface of cells, and this knowledge builds on my past work analyzing and characterizing glycans and related complex biologics. The same could be said for flu viruses like H5N1 and coronaviruses like SARS-CoV-2.
It is clear that once you have an outbreak, you must be able to combat the virus and quickly find a countermeasure. Many infectious diseases are also drug-resistant, as this is the natural way a pathogen evolves to escape and continue to survive. All these factors need to be put into a strategy for optimal drug development that is rapid, effective, and can prevent drug resistance. For these reasons, we have focused on the development of engineered antibodies that directly target the pathogen.
The approach we take at SMART is to use the regulatory framework as a design constraint. By starting with that framework in mind and working with the regulators each step of the way, we can rapidly develop, produce, and evaluate antibody candidates for safety and efficacy in humans.
Most recently, through Tychan, a biotech company founded by Professor Ooi Eng Eong and myself, we have developed in just four months the first monoclonal antibody (mAb) that targets SARS-CoV-2. Announced in June, this was the first clinical trial tackling the coronavirus in Singapore and it will evaluate the TY027 mAb regarding its safety and efficacy. Preliminary results from the phase 1 trials show that no adverse events have been observed after the infusion of TY027 in healthy volunteers.
First, we used computational methods to target functionally important, and evolutionarily stable, regions on the virus. Then our bioprocessing methods made antibodies in a matter of weeks, instead of the many months that are usually required if working with a master cell bank. Previously, we developed the world’s first anti-yellow fever virus antibody. Right now, this is in phase 2 clinical trials.
Q: Why is Singapore an ideal location to investigate these diseases?
A: I became involved at SMART after bird flu had been a big concern in Asia and countries like Singapore in particular. When you need to solve a problem, you need to get as close to its source as possible. I thought we should go to Singapore to understand how we can use our research to predict how the bird flu virus can gain a foothold in humans.
Singapore is now a leading biomedical sciences hub at the heart of Asia with world-class manufacturing capabilities and an extensive and integrated research ecosystem. At SMART, I can collaborate with local researchers who are not only familiar with the local issues but have also developed expertise in their fields.
In parallel, I became interested in how these viruses adapt to humans, and what effective countermeasures could be taken. We began developing a platform for antibody design, rather than using other established approaches. Our approach acknowledges that there are known structures and databases we actively use to very rapidly design, engineer and assemble antibodies to test in an iterative fashion. We then pick the best design to go forward and develop as a drug candidate.
In the case of infectious diseases like dengue and Zika, being at the source means that we can get a sense of the scale, scope, and seriousness of the problem or the outbreak when it appears around you. Dengue, for example, is endemic in Southeast Asia, while Zika first appeared in Brazil but eventually hit Singapore.
In Boston, saying dengue is important would be the furthest thing from people’s minds, but because of globalization and global warming, that’s likely to change. When you’re looking at dengue or bird flu that’s prevalent at that time, getting samples, and talking to clinician-scientists on the front line, you can learn the crucial nuances of the disease, its properties, and the gravity of an outbreak. Being armed with this information gives you the ability to move fast.
What’s more, the significance of the problem becomes much higher, the more you understand the implications of this disease; the farther away you are, the harder it is to grasp this significance. If you truly want to understand the issue, you need to be close to the source and grasp the elements that define what the problem statement is and what a pragmatic solution would be.
Q: What impact will the Covid-19 outbreak have on our approach to infectious disease therapeutics development?
A: Big pharmaceutical companies do not generally get involved in developing therapeutics for infectious diseases; instead, they tend to make huge investments in high-margin mass-market drugs, like cancer therapies. In infectious diseases, there is usually no mass market — though that is clearly not the case at the moment — and the drugs under development must also be accessible and affordable. Because of this, drugs for infectious diseases are not usually the sort of things the big companies will take on. It doesn’t help that outbreaks tend to be cyclical, so there is an urgent effort for developing a vaccine for an emerging infectious disease at one moment, then the crisis passes, and the need gets forgotten.
Consider antimicrobial resistance, which is an enormous global threat. Bacteria are learning to withstand the drugs that are used against them. Yet this is still not an exciting enough problem for pharmaceutical companies to invest in, compared to solving heart disease or the cancer problem.
I think Covid-19 is going to change the way these things are considered, given the significance of the economic and lifestyle impact it’s been having this year. We are still in the first wave and have months to go before any of the prospective solutions play out.
Covid-19 has hit at the core of national security for many influential countries. The pandemic has forced them to grapple with the idea that they might come under attack from another virus at any point, and they don’t want to be in a situation again of not being able to respond. The question that is ahead of us all is: How can we bring treatments for infectious diseases to market faster and more efficiently than we have done so far? It looks like we all have a lot more work to do.