Understanding how interactions between the central nervous system and the immune system contribute to problems of aging, including Alzheimer’s disease, Parkinson’s disease, arthritis, and more, can generate new leads for therapeutic development, speakers said at MIT’s symposium “The Neuro-Immune Axis and the Aging Brain” on Sept 18.
“The past decade has brought rapid progress in our understanding of how adaptive and innate immune systems impact the pathogenesis of neurodegenerative disorders,” said Picower Professor Li-Huei Tsai, director of The Picower Institute for Learning and Memory and MIT’s Aging Brain Initiative (ABI), in her introduction to the event, which more than 450 people registered to attend. “Together, today’s speakers will trace how the neuro-immune axis shapes brain health and disease … Their work converges on the promise of immunology-informed therapies to slow or prevent neurodegeneration and age-related cognitive decline.”

For instance, keynote speaker Michal Schwartz of the Weizmann Institute in Israel described her decades of pioneering work to understand the neuro-immune “ecosystem.” Immune cells, she said, help the brain heal, and support many of its functions, including its “plasticity,” the ability it has to adapt to and incorporate new information. But Schwartz’s lab also found that an immune signaling cascade can arise with aging that undermines cognitive function. She has leveraged that insight to investigate and develop corrective immunotherapies that improve the brain’s immune response to Alzheimer’s both by rejuvenating the brain’s microglia immune cells and bringing in the help of peripheral immune cells called macrophages. Schwartz has brought the potential therapy to market as the chief science officer of ImmunoBrain, a company testing it in a clinical trial.
In her presentation, Tsai noted recent work from her lab and that of computer science professor and fellow ABI member Manolis Kellis showing that many of the genes associated with Alzheimer’s disease are most strongly expressed in microglia, giving it an expression profile more similar to autoimmune disorders than to many psychiatric ones (where expression of disease-associated genes typically is highest in neurons). The study showed that microglia become “exhausted” over the course of disease progression, losing their cellular identity and becoming harmfully inflammatory.
“Genetic risk, epigenomic instability, and microglia exhaustion really play a central role in Alzheimer’s disease,” Tsai said, adding that her lab is now also looking into how immune T cells, recruited by microglia, may also contribute to Alzheimer’s disease progression.
The body and the brain
The neuro-immune “axis” connects not only the nervous and immune systems, but also extends between the whole body and the brain, with numerous implications for aging. Several speakers focused on the key conduit: the vagus nerve, which runs from the brain to the body’s major organs.
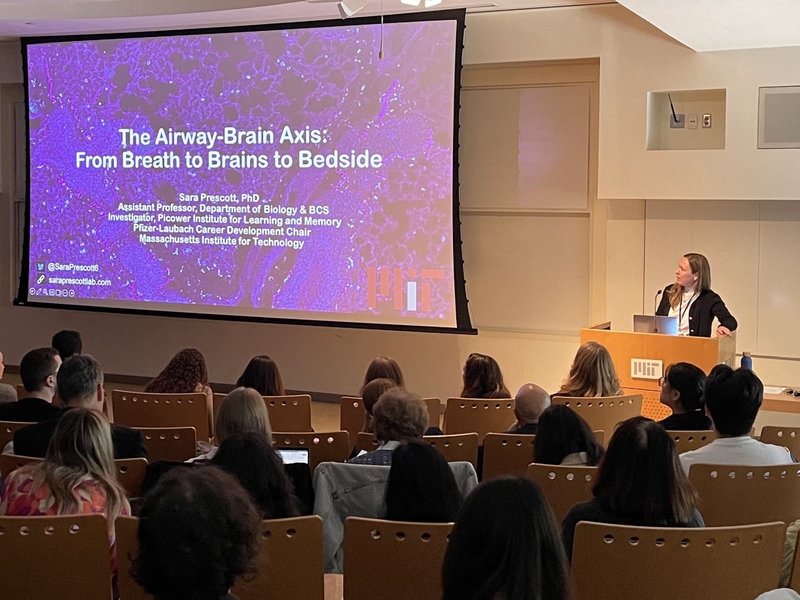
For instance, Sara Prescott, an investigator in the Picower Institute and an MIT assistant professor of biology, presented evidence her lab is amassing that the brain’s communication via vagus nerve terminals in the body’s airways is crucial for managing the body’s defense of respiratory tissues. Given that we inhale about 20,000 times a day, our airways are exposed to many environmental challenges, Prescott noted, and her lab and others are finding that the nervous system interacts directly with immune pathways to mount physiological responses. But vagal reflexes decline in aging, she noted, increasing susceptibility to infection, and so her lab is now working in mouse models to study airway-to-brain neurons throughout the lifespan to better understand how they change with aging.
In his talk, Caltech Professor Sarkis Mazmanian focused on work in his lab linking the gut microbiome to Parkinson’s disease (PD), for instance by promoting alpha-synuclein protein pathology and motor problems in mouse models. His lab hypothesizes that the microbiome can nucleate alpha-synuclein in the gut via a bacterial amyloid protein that may subsequently promote pathology in the brain, potentially via the vagus nerve. Based on its studies, the lab has developed two interventions. One is giving alpha-synuclein overexpressing mice a high-fiber diet to increase short-chain fatty acids in their gut, which actually modulates the activity of microglia in the brain. The high-fiber diet helps relieve motor dysfunction, corrects microglia activity, and reduces protein pathology, he showed. Another is a drug to disrupt the bacterial amyloid in the gut. It prevents alpha synuclein formation in the mouse brain and ameliorates PD-like symptoms. These results are pending publication.
Meanwhile, Kevin Tracey, professor at Hofstra University and Northwell Health, took listeners on a journey up and down the vagus nerve to the spleen, describing how impulses in the nerve regulate immune system emissions of signaling molecules, or “cytokines.” Too great a surge can become harmful, for instance causing the autoimmune disorder rheumatoid arthritis. Tracey described how a newly U.S. Food and Drug Administration-approved pill-sized neck implant to stimulate the vagus nerve helps patients with severe forms of the disease without suppressing their immune system.
The brain’s border
Other speakers discussed opportunities for understanding neuro-immune interactions in aging and disease at the “borders” where the brain’s and body’s immune system meet. These areas include the meninges that surround the brain, the choroid plexus (proximate to the ventricles, or open spaces, within the brain), and the interface between brain cells and the circulatory system.
For instance, taking a cue from studies showing that circadian disruptions are a risk factor for Alzheimer’s disease, Harvard Medical School Professor Beth Stevens of Boston Children’s Hospital described new research in her lab that examined how brain immune cells may function differently around the day-night cycle. The project, led by newly minted PhD Helena Barr, found that “border-associated macrophages” — long-lived immune cells residing in the brain’s borders — exhibited circadian rhythms in gene expression and function. Stevens described how these cells are tuned by the circadian clock to “eat” more during the rest phase, a process that may help remove material draining from the brain, including Alzheimer’s disease-associated peptides such as amyloid-beta. So, Stevens hypothesizes, circadian disruptions, for example due to aging or night-shift work, may contribute to disease onset by disrupting the delicate balance in immune-mediated “clean-up” of the brain and its borders.
Following Stevens at the podium, Washington University Professor Marco Colonna traced how various kinds of macrophages, including border macrophages and microglia, develop from the embryonic stage. He described the different gene-expression programs that guide their differentiation into one type or another. One gene he highlighted, for instance, is necessary for border macrophages along the brain’s vasculature to help regulate the waste-clearing cerebrospinal fluid (CSF) flow that Stevens also discussed. Knocking out the gene also impairs blood flow. Importantly, his lab has found that versions of the gene may be somewhat protective against Alzheimer’s, and that regulating expression of the gene could be a therapeutic strategy.
Colonna’s WashU colleague Jonathan Kipnis (a former student of Schwartz) also discussed macrophages that are associated with the particular border between brain tissue and the plumbing alongside the vasculature that carries CSF. The macrophages, his lab showed in 2022, actively govern the flow of CSF. He showed that removing the macrophages let Alzheimer’s proteins accumulate in mice. His lab is continuing to investigate ways in which these specific border macrophages may play roles in disease. He’s also looking in separate studies of how the skull’s brain marrow contributes to the population of immune cells in the brain and may play a role in neurodegeneration.

For all the talk of distant organs and the brain’s borders, neurons themselves were never far from the discussion. Harvard Medical School Professor Isaac Chiu gave them their direct due in a talk focusing on how they participate in their own immune defense, for instance by directly sensing pathogens and giving off inflammation signals upon cell death. He discussed a key molecule in that latter process, which is expressed among neurons all over the brain.
Whether they were looking within the brain, at its border, or throughout the body, speakers showed that age-related nervous system diseases are not only better understood but also possibly better treated by accounting not only for the nerve cells, but their immune system partners.