Many of our body’s most important functions occur without our conscious knowledge, such as digestion, heartbeat, and breathing. These vital functions depend on the signals generated by the “interoceptive nervous system,” which enables the brain to monitor our internal organs and trigger responses that sometimes save our lives. One second you are breathing normally as you eat your salad and the next, when a vinegar-soaked crouton enters your throat, you are coughing or swallowing to protect and clear your airway. We know our bodies are sensitive to cues like irritants, but we still have a lot to learn about how the interoceptive system works to meet our physiological needs, keep organs safe and healthy, and affect our behavior. We can also learn how chronic insults may lead to organ dysfunction and use what we learn to create therapeutic interventions.
Focusing on the airway, Sara Prescott, a new faculty member in the Department of Biology and investigator in The Picower Institute for Learning and Memory, seeks to understand the ways our nervous systems detect and respond to stimuli in health and disease. Here, she describes her work.
Q: Why is understanding the peripheral nervous system important, and what parts of your background are you drawing on for your current research?
A: The lab focuses on really trying to explore the body-brain connection.
People often think that our mind exists in a vacuum, but in reality, our nervous system is heavily integrated with the rest of the body, and those neural interfaces are important, both for taking information from our body or environment and turning it into an internal representation of the world, and, in reverse, being able to process that information and being able to enact changes throughout the body. That includes things like autonomic reflexes, basic functions of the body like breathing, blood-gas regulation, digestion, and heart rate.
I’ve integrated both my graduate training and postdoctoral training into thinking about biology across multiple scales.
Graduate school for me was quite focused on deep molecular mechanism questions, particularly gene regulation, so I feel like that has been very useful for me in my general approach to neuroscience because I take a very molecular angle to all of this.
It also showed me the power of in vitro models as reductionist tools to explore fundamental aspects of cell biology. During my postdoc, I focused on larger, emergent phenotypes. We were able to manipulate specific circuits and see very impressive behavioral responses in animals. You could stimulate about 100 neurons in a mouse and see that their breathing would just stop until you remove the stimulation, and then the breathing would return to normal.
Both of those experiences inform how we approach a problem in my research. We need to understand how these circuits work, not just their connectivity at the anatomical level but what is driving their changes in sensitivity over time, the receptor expression programs that affect how they sense and signal, how these circuits emerge during development, and their gene expression.
There are still so many foundational questions that haven’t been answered that there’s enough to do in the mouse for quite some time.
Q: How are you specifically looking into interoceptive biology at MIT?
A: Our flagship system is the mammalian airway. We use a mouse model and modern molecular neuroscience tools to manipulate various neural pathways and observe what the effects are on respiratory function and animal health.
Neuroscience and mouse work have a reputation for being a little challenging and intense, but I think this is also where we can ask really important questions that are useful for our everyday lives — and the only place where we can fully recapitulate the complexity of nervous system signaling all the way down to our organs, back to our brain, and back to our organs.
It’s a very fun place to do science with lots of open questions.
One of the core discoveries from my postdoctoral work was focusing on the vagus nerve as a major body-to-brain conduit, as it innervates our lungs, heart, and gastrointestinal tract. We found that there were about 40 different subtypes of sensory neurons within this small nerve, which is really a remarkable amount of diversity and reflects the massive sensory space within the body. About a dozen of those vagal neurons project to the airways.
We identified a rare neuron type specifically responsible for triggering protective responses, like coughing when water or acid entered the airway. We also discovered a separate population of neurons that make us feel and act sick when we get a flu infection. The field now knows what four to five vagal populations of neurons are actually sensing in the airways, but the remaining populations are still a mystery to us; we don’t know what those populations of sensory neurons are detecting, what their anatomy is, and what reflex effects those neurons are evoking.
Looking ahead, there are many exciting directions for the interoceptive biology field. For example, there’s been a lot of focus on characterizing the circuits underlying acute motor reflexes, like rapid responses to visceral stimuli on the timescale of minutes to hours. But we don’t have a lot of information about what happens when these circuits are activated over long periods of time. For example, respiratory tract infections often last for weeks or longer. We know that the airways undergo changes in composition when they’re exposed to different types of infection or stress to better accommodate future threats. One of the hypotheses we’re testing is that chronically activating neural circuits may drive changes in organ composition. We have this idea, which we’re calling reflexive remodeling: neurons may be communicating with stem cells and progenitor cells in the periphery to drive adaptive remodeling responses.
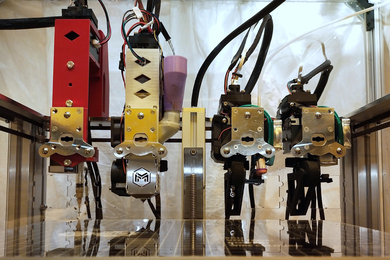
We have the genetic, molecular, and circuit scale tools to explore this phenomenon in mice. In parallel, we’re also setting up some in vitro models of the mouse airway mucosa to expedite receptor screening and to explore basic mechanisms of neuron-epithelium cross-talk. We hope this will inform our understanding of how the airway surface senses and responds to different types of irritants or damage.
Q: This all sounds fascinating. Where does it lead?
A: Human health has been my north star for a long time and I’ve taken a long, wandering path to find particular areas where I can scratch whatever intellectual itch that I have.
I originally thought I would be a doctor and then realized that I felt like I could have a more lasting impact by discovering fundamental truths about how our bodies work. I think there are a number of chronic diseases in which autonomic imbalance is actually a huge clinical component of the disorder.
We have a lot of interest in some of these very common airway remodeling diseases, like chronic obstructive pulmonary disorder — COPD — asthma, and potentially lung cancer. We want to ask questions like how autonomic circuits are altered in disease contexts, and when neurons actually drive features of disease.
Perhaps this research will help us come up with better molecular, cellular, or tissue engineering approaches to improve the outcomes for a variety of autonomic diseases.
It’s very easy for me to imagine how one day, not too far from now, we can turn these findings into something actionable for human health.