Hundreds of millions of people worldwide suffer from a vision condition called amblyopia, or lazy eye, with imbalanced vision in their two eyes. Unless this disabling condition is caught and treated at a young age, it's rare for children to regain full vision, because the brain learns to turn off the input from the “lazy” eye.
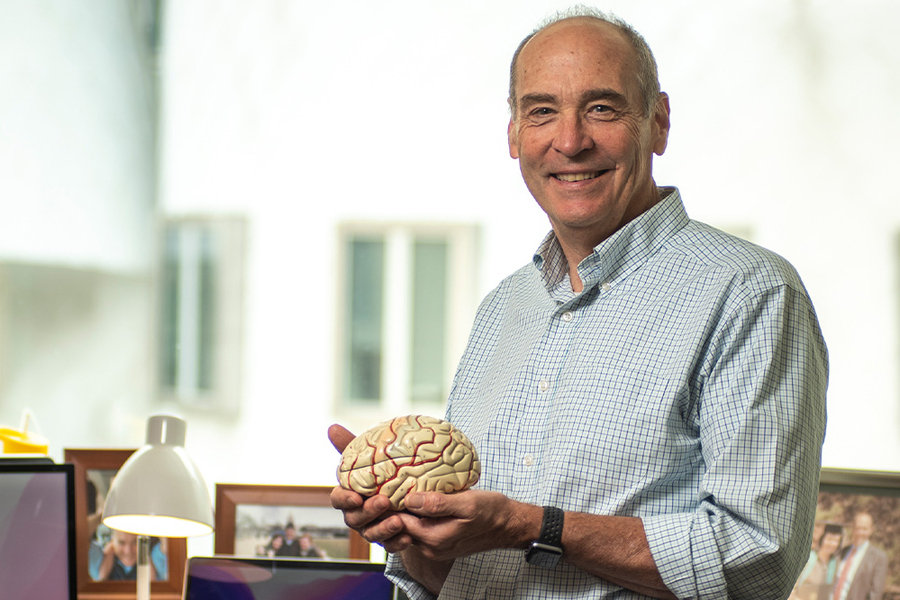
Amblyopia is one striking example of how the brain is modified by experience, says Professor Mark Bear, a neuroscientist at MIT's Picower Institute for Learning and Memory. His research focuses on this phenomenon of brain plasticity, with particular attention to the synapses that connect neurons in the brain.
Bear's studies have led to a potential treatment for amblyopia that works by temporarily anesthetizing the “good” eye. After successful experiments in smaller animals, the method is being tested in non-human primates, and Bear and his partners hope to move ahead into clinical trials.
Wiring up our vision
“Consider the challenge of seeing one world through two eyes,” Bear suggests. To avoid seeing double, information from the two retinas must be mapped with extreme precision onto common targets in the brain. But we're not born with this ability; it depends on high-quality visual experience during infancy and early childhood.
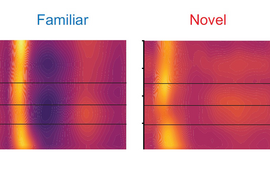
This need for the brain to learn to see fully was demonstrated decades ago, in experiments with young animals with a patch placed over one eye. When the patch was removed, researchers discovered a severe visual impairment through the eye that had been patched. “The retina was fine,” he says. “The problem was that it had been mis-wired in the brain, so that these connections didn't mature normally.”
The finding raised fascinating scientific questions, Bear says. How have the brain's synaptic connections been modified? What triggers these modifications? And how might those connections recover?
“Today we can trace the whole path that goes from poor-quality visual experience to poor quality-of-vision and visual impairment in the brain,” he says. Research has demonstrated that the condition is triggered by replacing well-correlated activity in the retinas with retinal noise. “That type of activity weakly activates a particular neurotransmitter receptor in the brain called an NMDA receptor, which triggers the modification of synapses that causes those synapses to get weaker,” he says.
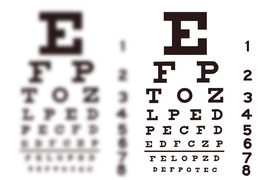
These findings have practical implications for the vast number of children born with amblyopia, usually due to one of three causes. Their eyes may be cross-eyed, or they may be born with a cataract in one eye, or the two eyes refract (focus) differently so that they only view the world crisply through one eye or the other. All of these mishaps disrupt the wiring of the brain, resulting in poor visual acuity in one eye and loss of binocular vision, says Bear.
The current medical treatment is simply to put a patch over the good eye, to try to force relearning of vision through the weak eye. This procedure can work but is rarely completely successful. And it must begin early — in the first year for children with cataracts, perhaps at the age of 7 or 8 years for less severe causes of the condition.
Amblyopia is particularly devastating for people who later lose use of their good eye. But in a surprising number of cases, the amblyopic eye then does recover some vision, even in adults. “That means there is plasticity in the adult brain, which is good,” Bear says.
So what drives this recovery, when patching the good eye doesn't work? Bear and his colleagues hypothesized that patches don't work because the retina remains very active in the dark behind the patch.
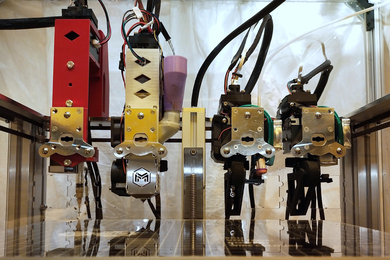
“To test our hypothesis, you would like to completely inactivate the retina,” he says. His team did just that by injecting a long-lasting anesthetic called tetrodotoxin (TTX) directly into the eye of lab animals that model severe amblyopia.
“We see, quite remarkably, a very dramatic and surprisingly rapid recovery of vision to the amblyopic eye,” says Bear. “It can be complete recovery of vision. And when the TTX wears off, the good eye comes bounding right back, so we're able to reverse amblyopia in adult animals.”
Bear and his collaborators are beginning experiments in non-human primates, where the procedure seems to be safe, but they don't yet have results on how effective the method is.
He's also working with clinician scientists “who see patients with amblyopia and understand the toll that it takes on these patients and their families,” he says. And he's begun early conversations with potential commercial partners to support a move into clinical studies.
Figuring Fragile X syndrome
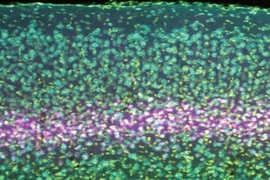
Another major effort in Bear's lab focuses on understanding Fragile X syndrome. This is a genetic disorder caused by the deletion of a single gene and the most common heritable form of intellectual disability and autism.
Two decades ago, his lab made an important discovery about the protein product of that lost single gene, which “put Fragile X on the map as a potentially interesting disease area for treatments,” he says.
The discovery led to a round of clinical trials that proved disappointing, but the Bear lab is among many around the world further investigating Fragile X biology and coming up with promising new approaches to treat the condition.
The Holy Grail for these efforts would be a way to re-express the protein that has gone missing, but other treatments also might eventually ameliorate various effects of Fragile X syndrome. “We won’t reverse the effects of growing up with Fragile X in an adult, but we should be able to greatly improve the quality of life for those affected by the disease,” he says.
Bringing MIT brainpower to the brain
The Picower Institute, one major group in MIT's world-leading Department of Brain and Cognitive Sciences, “is a wonderful place to do science,” Bear says. “It is an embarrassment of riches. My heart rate goes up every time I arrive on campus, just thinking about what's going on around me. It's almost frustrating, like going to an ice cream shop with 100 different flavors of ice cream. There's so much going on; I have to choose wisely.”
Bear hopes that deepening understanding of brain plasticity in his lab and others around the globe will pay off in the not-too-distant future for patients with disabling conditions such as amblyopia and Fragile X syndrome.
“Basic scientists take satisfaction in doing basic science,” he adds. “If there was never an application of my work, I would still die a happy man. But there would be nothing sweeter than to have something we discovered in the lab lead to some improvement in the human condition.”