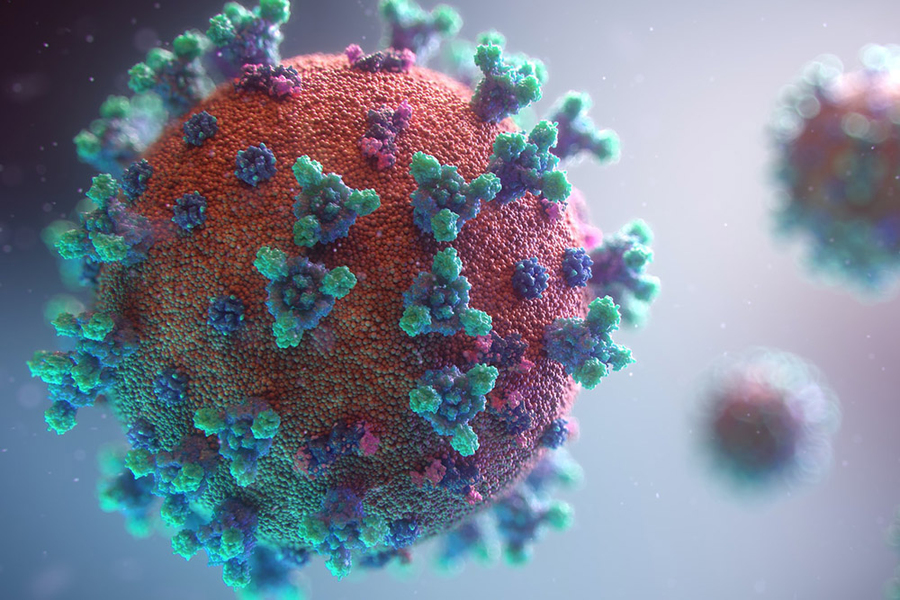
Researchers from Critical Analytics for Manufacturing Personalized-Medicine (CAMP), an interdisciplinary research group at the Singapore-MIT Alliance for Research and Technology (SMART), MIT’s research enterprise in Singapore, have developed a new method for rapid and accurate detection of viral nucleic acids — a breakthrough that can be easily adapted to detect different DNA/RNA targets in viruses like the coronavirus.
The pandemic has highlighted the importance of rapid diagnostics and improved methods to detect viruses, especially as the world seeks to be prepared for future pandemics or the next dangerous pathogen. Particularly, the biomanufacturing industry, with the unique challenges of using cells as cell therapy products, is looking for innovations in rapid methods to detect virus contamination as part of their quality control processes and in release testing. While the reverse transcription-quantitative polymerase chain reaction (RT-qPCR) is considered a gold standard for viral detection, there are limitations and they can often produce variable results.
A more accurate version is the digital PCR method that allows absolute quantification (meaning it reveals the copy number of viruses in a sample), can allow for setting clear thresholds of virus contamination, and is not susceptible to potential fluctuations of reference gene required by standard qPCR methods. However, digital PCR demands a relatively long reaction time of around four hours. Another drawback of all current PCR-based methods is that they need expensive equipment for precise temperature control and cycling.
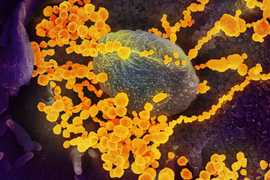
The new methodological development by CAMP — the RApid DIgital Crispr Approach (RADICA) — allows absolute quantification of viral nucleic acids in 40-60 minutes in an isothermal manner in a water bath, a prototypical and inexpensive laboratory equipment. The team’s research is explained in a paper titled “Digital CRISPR-based method for the rapid detection and absolute quantification of nucleic acids” published recently in the journal Biomaterials.
The RADICA method has been tested on SARS-CoV-2 synthetic DNA/RNA as well as the Epstein-Barr virus in cultured B cells and patient serum. The researchers say the method can be adapted to detect other kinds of viruses, and in other types of samples such as saliva and cell culture media. RADICA is also able to distinguish the viruses from their close relatives.
“This is the first reported method of detecting nucleic acids to utilize the sensitivity of isothermal amplification and specificity of CRISPR-based detection in a digital format — allowing rapid and specific amplification of DNA without the time-consuming and costly need for thermal cycling,” says Xiaolin Wu, a postdoc at SMART CAMP. “RADICA offers four times faster absolute quantification compared to conventional digital PCR methods.”
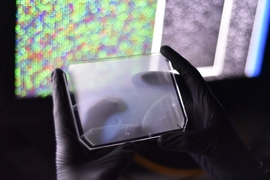
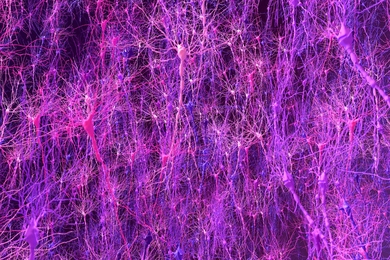
The team uses extracted DNA/RNA of the sample and divides a 15 microliter reaction into thousands of independent partitions. In each partition, the DNA/RNA is amplified and identified by Cas12a protein, an enzyme that can turn the target signal into a fluorescent signal. This allows absolute quantification to be achieved by counting the number of partitions that have the target DNA/RNA and are lit up.
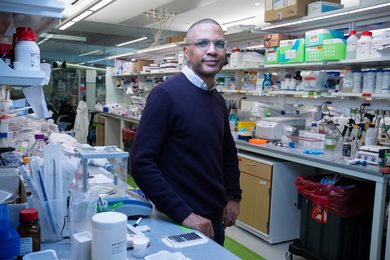
“The last year has shown us the importance of detecting viruses quickly and accurately, and RADICA can help fill existing gaps in this area,” says National University of Singapore Professor Hanry Yu, co-corresponding author and co-lead principal investigator at SMART CAMP. “Cell therapy products have a very short shelf life, and patients are usually in need of treatment urgently. Current sterility tests need around 14 days, which is too slow for clinical needs, but RADICA shortens the process into hours.”
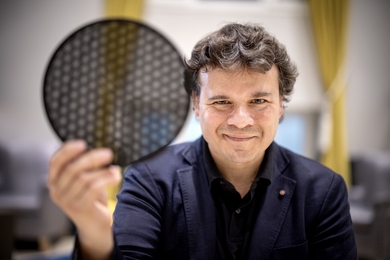
Timothy Lu, who is co-corresponding author, CAMP principal investigator, and associate professor of biological engineering and electrical engineering and computer science at MIT, says the team’s method is faster, cheaper, and more efficient than what is used today, and its digital format makes it more tolerant to contamination or inhibitors that may be present in biological samples — often the case with cell therapy products. Lu adds that on top of detecting the presence of a target virus, RADICA also identifies how many viruses there are in the sample, which can help doctors and researchers in deciding the course of treatment, as well as production and inventory management of cell therapy products.
While the researchers at CAMP developed RADICA for monitoring cell therapy manufacturing processes and biosafety release testing of cell therapy products, Wu says the method can also be used to detect DNA/RNA targets of different viruses and adapted to devices commonly found in hospitals and service laboratories — providing a potential new way to tackle pandemics.
The research is carried out by SMART and supported by the National Research Foundation (NRF) Singapore under its Campus for Research Excellence And Technological Enterprise (CREATE) program.
CAMP was launched in June 2019. It focuses on better ways to produce living cells as medicine or cellular therapies, to provide more patients access to promising and approved therapies. The investigators at CAMP address two key bottlenecks facing the production of a range of potential cell therapies: critical quality attributes (CQA) and process analytic technologies (PAT). Leveraging deep collaborations within Singapore and MIT, CAMP invents and demonstrates CQA/PAT capabilities from stem to immune cells. Its work addresses ailments ranging from cancer to tissue degeneration, targeting adherent and suspended cells, with and without genetic engineering.
CAMP is the R&D core of a comprehensive national effort on cell therapy manufacturing in Singapore.
SMART was established by MIT in partnership with the NRF in 2007. SMART, the first entity in CREATE, serves as an intellectual and innovation hub for research interactions between MIT and Singapore, undertaking cutting-edge research in areas of interest to both. SMART currently comprises an Innovation Center and interdisciplinary research groups: Antimicrobial Resistance, CAMP, Disruptive and Sustainable Technologies for Agricultural Precision, Future Urban Mobility, and Low Energy Electronic Systems.