Waiting to see a doctor is frustrating, as anyone who has spent too much time flipping through old magazines or warily eyeing coughing strangers can attest. According to a new study by MIT researchers, Medicaid patients experience more of this frustration than people with private health insurance.
Consider: Medicaid recipients are 20 percent more likely to wait more than 20 minutes to begin a scheduled appointment, compared to privately insured patients. The median wait time of Medicaid enrollees is longer as well. As the findings show, much — but not all — of this disparity is because Medicaid patients tend to use providers who generally have longer wait times for their patients.
The results shed new light on the full range of experiences people have with the health care system, even apart from treatment outcomes.
“People want to focus on health care quality, but if you’ve ever had any experience with the health care system, you know there are a lot of nonhealth amenities associated with your visit,” says Amy Finkelstein, the John and Jennie S. MacDonald Professor of Economics at MIT and co-author of a newly published paper that details the results of the study.
The study uses the issue of wait times to compare the quality of health care access provided through public means, such as Medicaid, and through private insurance.
“It’s a different way of looking at an older problem,” says Tamar Oostrom, a doctoral candidate in MIT’s Department of Economics, who is the lead author of the new paper.
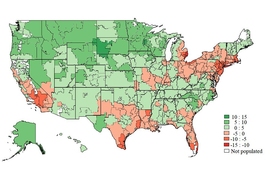
The study also uncovered a variety of new findings about differences in wait times. For instance, wait times are generally shorter in the mornings, as well as in larger medical practices. People spend less time waiting for doctors in New England than in any other region of the country. And here’s a data point that may reassure some harried parents: Young children are late for 40 percent of their medical visits.
The paper, “Outpatient Office Wait Times And Quality of Care for Medicaid Patients,” is being published today in the journal Health Affairs. The authors are Oostrom, Finkelstein, and Liran Einav, a professor in the Department of Economics at Stanford University.
The researchers examined 21.4 million anonymized records from athenahealth, the electronic records provider. The data cover all outpatient visits the firm processed in 2013, from 2,581 different medical practices. Wait time was measured based on information the athenahealth software captures showing the patient’s arrival and check-in times, the scheduled appointment time, and the time when the “intake” phase of the visit begins.
The study accounted for varying characteristics of both providers and the nature of the medical visits. This approach allowed the researchers to determine that most of the variation in waiting time, between Medicaid patients and privately insured patients, is attributable to the type of provider in question.
“Most of this difference in wait times is explained by the practices and providers Medicaid recipients see,” Oostrom says. There may be many reasons for this: For instance, Medicaid patients may be more likely to visit providers with larger loads of patients in the first place, making delays more likely.
And yet, even when adjusting for the type of provider, Medicaid patients still wait 5 percent longer than patients with private insurance, something the researchers regard as difficult to interpret. In the paper, they suggest this could reflect “triaging of patients by insurance status within an office.” Medicaid patients also face more pronounced delays in states with less extensive Medicaid reimbursement policies.
All told, the average wait times were 4.1 minutes for patients with private insurance and 4.6 minutes for patients enrolled in Medicaid. Finkelstein, for one, acknowledges she was surprised by those figures.
“My intuition, going into it, was that wait times were going to be much longer, based on my own biased recall,” she says. “We tend to remember that visit where we waited forever. A key value of measuring wait times based on information captured by office software is it doesn’t suffer from such biased recall.”
That said, Finkelstein adds, she was not surprised to see some of the more specific results, such as the fact that families with young children are so frequently running late to their appointments.
In the past, Finkelstein has collaborated with several other researchers on groundbreaking studies about Medicaid, the health care insurance program that often gives coverage to low-income citizens and is funded by both the federal government and states. Her research has shown that newly enrolled Medicaid patients make more trips overall to providers after acquiring insurance, make more visits to emergency rooms, and benefit financially from having insurance, among other findings.
The current study could open up new questions about the influence of the overall experience during health care visits. Future research could explore how negative perceptions of wait times affect the willingness of patients to seek more care. And the study bears on what researchers call the “opportunity cost” of visiting the doctor — that is, the fact that patients often have to take time out from their jobs to receive health care.
“I hope this is the tip of the iceberg for us and others in trying to think about the nonhealth amenities in the health care system,” Finkelstein says.



![“Contrary to the conjecture that Medicaid would get people to [move] out of the emergency room and to the primary care physician, we’re seeing a persistent increase in emergency room use,” says Amy Finkelstein, the John and Jennie S. MacDonald Professor of Economics at MIT.](/sites/default/files/styles/news_article__archive/public/images/201610/MIT-amy-finkelstein.jpg?itok=HeXLwtW1)