Audio
Immune molecules called cytokines play important roles in the body’s defense against infection, helping to control inflammation and coordinating the responses of other immune cells. A growing body of evidence suggests that some of these molecules also influence the brain, leading to behavioral changes during illness.
Two new studies from MIT and Harvard Medical School, focused on a cytokine called IL-17, now add to that evidence. The researchers found that IL-17 acts on two distinct brain regions — the amygdala and the somatosensory cortex — to exert two divergent effects. In the amygdala, IL-17 can elicit feelings of anxiety, while in the cortex it promotes sociable behavior.
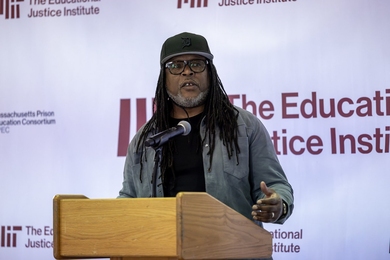
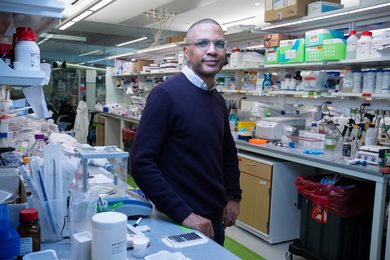
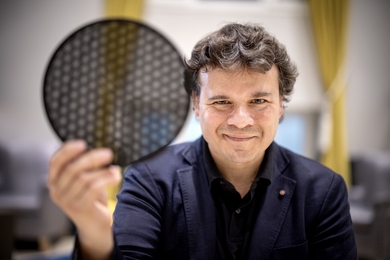
These findings suggest that the immune and nervous systems are tightly interconnected, says Gloria Choi, an associate professor of brain and cognitive sciences, a member of MIT’s Picower Institute for Learning and Memory, and one of the senior authors of the studies.
“If you’re sick, there’s so many more things that are happening to your internal states, your mood, and your behavioral states, and that’s not simply you being fatigued physically. It has something to do with the brain,” she says.
Jun Huh, an associate professor of immunology at Harvard Medical School, is also a senior author of both studies, which appear today in Cell. One of the papers was led by Picower Institute Research Scientist Byeongjun Lee and former Picower Institute research scientist Jeong-Tae Kwon, and the other was led by Harvard Medical School postdoc Yunjin Lee and Picower Institute postdoc Tomoe Ishikawa.
Behavioral effects
Choi and Huh became interested in IL-17 several years ago, when they found it was involved in a phenomenon known as the fever effect. Large-scale studies of autistic children have found that for many of them, their behavioral symptoms temporarily diminish when they have a fever.
In a 2019 study in mice, Choi and Huh showed that in some cases of infection, IL-17 is released and suppresses a small region of the brain’s cortex known as S1DZ. Overactivation of neurons in this region can lead to autism-like behavioral symptoms in mice, including repetitive behaviors and reduced sociability.
“This molecule became a link that connects immune system activation, manifested as a fever, to changes in brain function and changes in the animals’ behavior,” Choi says.
IL-17 comes in six different forms, and there are five different receptors that can bind to it. In their two new papers, the researchers set out to map which of these receptors are expressed in different parts of the brain. This mapping revealed that a pair of receptors known as IL-17RA and IL-17RB is found in the cortex, including in the S1DZ region that the researchers had previously identified. The receptors are located in a population of neurons that receive proprioceptive input and are involved in controlling behavior.
When a type of IL-17 known as IL-17E binds to these receptors, the neurons become less excitable, which leads to the behavioral effects seen in the 2019 study.
“IL-17E, which we’ve shown to be necessary for behavioral mitigation, actually does act almost exactly like a neuromodulator in that it will immediately reduce these neurons’ excitability,” Choi says. “So, there is an immune molecule that’s acting as a neuromodulator in the brain, and its main function is to regulate excitability of neurons.”
Choi hypothesizes that IL-17 may have originally evolved as a neuromodulator, and later on was appropriated by the immune system to play a role in promoting inflammation. That idea is consistent with previous work showing that in the worm C. elegans, IL-17 has no role in the immune system but instead acts on neurons. Among its effects in worms, IL-17 promotes aggregation, a form of social behavior. Additionally, in mammals, IL-17E is actually made by neurons in the cortex, including S1DZ.
“There’s a possibility that a couple of forms of IL-17 perhaps evolved first and foremost to act as a neuromodulator in the brain, and maybe later were hijacked by the immune system also to act as immune modulators,” Choi says.
Provoking anxiety
In the other Cell paper, the researchers explored another brain location where they found IL-17 receptors — the amygdala. This almond-shaped structure plays an important role in processing emotions, including fear and anxiety.
That study revealed that in a region known as the basolateral amygdala (BLA), the IL-17RA and IL-17RE receptors, which work as a pair, are expressed in a discrete population of neurons. When these receptors bind to IL-17A and IL-17C, the neurons become more excitable, leading to an increase in anxiety.
The researchers also found that, counterintuitively, if animals are treated with antibodies that block IL-17 receptors, it actually increases the amount of IL-17C circulating in the body. This finding may help to explain unexpected outcomes observed in a clinical trial of a drug targeting the IL-17-RA receptor for psoriasis treatment, particularly regarding its potential adverse effects on mental health.
“We hypothesize that there’s a possibility that the IL-17 ligand that is upregulated in this patient cohort might act on the brain to induce suicide ideation, while in animals there is an anxiogenic phenotype,” Choi says.
During infections, this anxiety may be a beneficial response, keeping the sick individual away from others to whom the infection could spread, Choi hypothesizes.
“Other than its main function of fighting pathogens, one of the ways that the immune system works is to control the host behavior, to protect the host itself and also protect the community the host belongs to,” she says. “One of the ways the immune system is doing that is to use cytokines, secreted factors, to go to the brain as communication tools.”
The researchers found that the same BLA neurons that have receptors for IL-17 also have receptors for IL-10, a cytokine that suppresses inflammation. This molecule counteracts the excitability generated by IL-17, giving the body a way to shut off anxiety once it’s no longer useful.
Distinctive behaviors
Together, the two studies suggest that the immune system, and even a single family of cytokines, can exert a variety of effects in the brain.
“We have now different combinations of IL-17 receptors being expressed in different populations of neurons, in two different brain regions, that regulate very distinct behaviors. One is actually somewhat positive and enhances social behaviors, and another is somewhat negative and induces anxiogenic phenotypes,” Choi says.
Her lab is now working on additional mapping of IL-17 receptor locations, as well as the IL-17 molecules that bind to them, focusing on the S1DZ region. Eventually, a better understanding of these neuro-immune interactions may help researchers develop new treatments for neurological conditions such as autism or depression.
“The fact that these molecules are made by the immune system gives us a novel approach to influence brain function as means of therapeutics,” Choi says. “Instead of thinking about directly going for the brain, can we think about doing something to the immune system?”
The research was funded, in part, by Jeongho Kim and the Brian Impact Foundation Neuro-Immune Fund, the Simons Foundation Autism Research Initiative, the Simons Center for the Social Brain, the Marcus Foundation, the N of One: Autism Research Foundation, the Burroughs Wellcome Fund, the Picower Institute Innovation Fund, the MIT John W. Jarve Seed Fund for Science Innovation, Young Soo Perry and Karen Ha, and the National Institutes of Health.