As the brain processes information, electrical charges zip through its circuits and neurotransmitters pass molecular messages from cell to cell. Both forms of communication are vital, but because they are usually studied separately, little is known about how they work together to control our actions, regulate mood, and perform the other functions of a healthy brain.
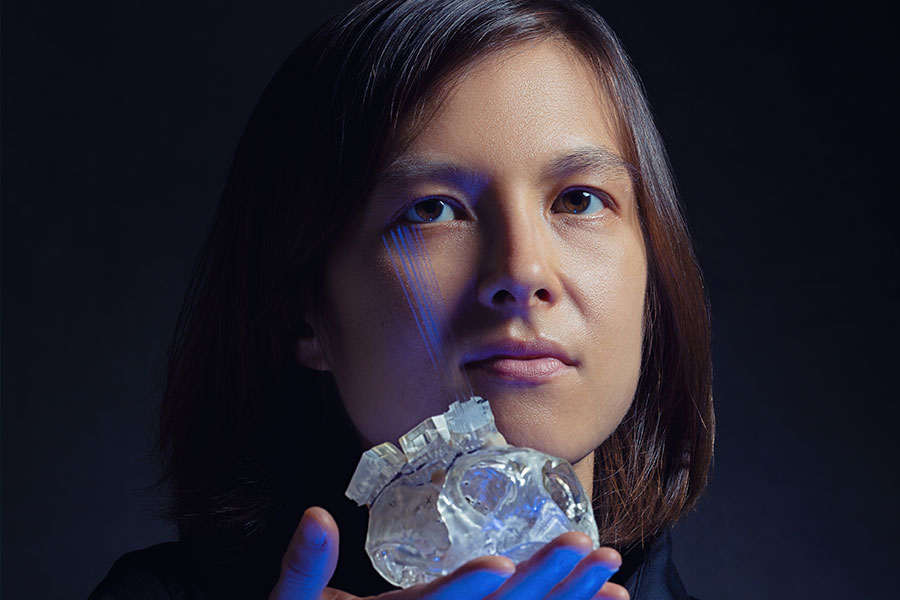
Neuroscientists in Ann Graybiel’s laboratory at MIT’s McGovern Institute for Brain Research are taking a closer look at the relationship between these electrical and chemical signals. “Considering electrical signals side by side with chemical signals is really important to understand how the brain works,” says Helen Schwerdt, a postdoc in Graybiel’s lab. Understanding that relationship is also crucial for developing better ways to diagnose and treat nervous system disorders and mental illness, she says, noting that the drugs used to treat these conditions typically aim to modulate the brain’s chemical signaling, yet studies of brain activity are more likely to focus on electrical signals, which are easier to measure.
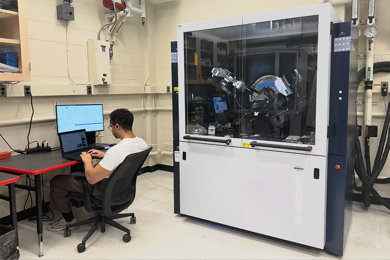
Schwerdt and colleagues in Graybiel’s lab have developed new tools so that chemical and electrical signals can, for the first time, be measured simultaneously in the brains of primates. In a study published Sept. 25 in Science Advances, they used those tools to reveal an unexpectedly complex relationship between two types of signals that are disrupted in patients with Parkinson’s disease — dopamine signaling and coordinated waves of electrical activity known as beta-band oscillations.
Complicated relationship
Graybiel’s team focused its attention on beta-band activity and dopamine signaling because studies of patients with Parkinson’s disease had suggested a straightforward inverse relationship between the two. The tremors, slowness of movement, and other symptoms associated with the disease develop and progress as the brain’s production of the neurotransmitter dopamine declines, and, at the same time, beta-band oscillations surge to abnormal levels. Beta-band oscillations are normally observed in parts of the brain that control movement when a person is paying attention or planning to move. It’s not clear what they do or why they are disrupted in patients with Parkinson’s disease. But because patients’ symptoms tend to be worst when beta activity is high — and because beta activity can be measured in real time with sensors placed on the scalp or with a deep-brain stimulation device that has been implanted for treatment, researchers have been hopeful that it might be useful for monitoring the disease’s progression and patients’ response to treatment. In fact, clinical trials are already underway to explore the effectiveness of modulating deep-brain stimulation treatment based on beta activity.
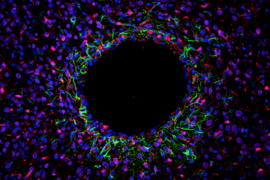
When Schwerdt and colleagues examined these two types of signals in the brains of rhesus macaques, they discovered that the relationship between beta activity and dopamine is more complicated than previously thought. Their new tools allowed them to simultaneously monitor both signals with extraordinary precision, targeting specific parts of the striatum — a region deep within the brain involved in controlling movement, where dopamine is particularly abundant — and taking measurements on the millisecond time scale to capture neurons’ rapid-fire communications.
They took these measurements as the monkeys performed a simple task, directing their gaze in a particular direction in anticipation of a reward. This allowed the researchers to track chemical and electrical signaling during the active, motivated movement of the animals’ eyes. They found that beta activity did increase as dopamine signaling declined — but only in certain parts of the striatum and during certain tasks. The reward value of a task, an animal’s past experiences, and the particular movement the animal performed all impacted the relationship between the two types of signals.
“What we expected is there in the overall view, but if we just look at a different level of resolution, all of a sudden the rules don’t hold,” says Graybiel, who is an MIT Institute Professor. “It doesn’t destroy the likelihood that one would want to have a treatment related to this presumed opposite relationship, but it does say there’s something more here that we haven’t known about.”
The researchers say it’s important to investigate this more nuanced relationship between dopamine signaling and beta activity, and that understanding it more deeply might lead to better treatments for patients with Parkinson’s disease and related disorders. While they plan to continue to examine how the two types of signals relate to one another across different parts of the brain and under different behavioral conditions, they hope that other teams will also take advantage of the tools they have developed. “As these methods in neuroscience become more and more precise and dazzling in their power, we’re bound to discover new things,” says Graybiel.
Joining Graybiel and Schwerdt on the study are Michael Cima, the David H. Koch Professor of Engineering in the Department of Materials Science and Engineering and a member of MIT’s Koch Institute for Integrative Cancer Research; Robert Langer, the David H. Koch Institute Professor and a member of the Koch Institute; Robert Desimone, director of the McGovern Institute; MIT research scientists Ken Amemori, Dan Gibson, Narcisse Bichot, Satoko Amemori; and Graybiel lab technicians Lauren Stanwicks and Tomoko Yoshida.
This study was supported by the National Institute of Biomedical Imaging and Bioengineering, the National Institute of Neurological Disorders and Stroke, the U.S. Army Research Office, the Saks Kavanaugh Foundation, the National Science Foundation, Kristin R. Pressman and Jessica J. Pourian ’13 Fund, and Robert Buxton.