Many Covid-19 patients who have been treated for weeks or months with mechanical ventilation have been slow to regain consciousness even after being taken off sedation. A new article in the Proceedings of the National Academy of Sciences offers the hypothesis that this peculiar response could be the effect of a hibernation-like state invoked by the brain to protect cells from injury when oxygen is scarce.
A very similar kind of state, characterized by the same signature change of brain rhythms, is not only observed in cardiac arrest patients treated by chilling their body temperature, a method called “hypothermia,” but also by the painted turtle, which has evolved a form of self-sedation to contend with long periods of oxygen deprivation, or “anoxia,” when it overwinters underwater.
“We propose that hypoxia combined with certain therapeutic maneuvers may initiate an as-yet-unrecognized protective down-regulated state (PDS) in humans that results in prolonged recovery of consciousness in severe Covid-19 patients following cessation of mechanical ventilation and in post-cardiac arrest patients treated with hypothermia,” wrote authors Nicholas D. Schiff and Emery N. Brown. “In severe Covid-19 patients we postulate that the specific combination of intermittent hypoxia, severe metabolic stress and GABA-mediated sedation may provide a trigger for the PDS.”
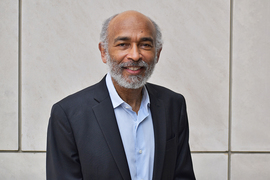
Schiff is a Jerold B. Katz Professor of Neurology and Neuroscience in the Feil Family Brain Mind Research Institute at Weill Cornell Medicine. Brown is the Edward Hood Taplin Professor of Medical Engineering and Computational Neuroscience in The Picower Institute for Learning and Memory and the Institute for Medical Engineering and Science at MIT. He is also an anesthesiologist at Massachusetts General Hospital and the Warren M. Zapol Professor of Anaesthesia at Harvard Medical School.
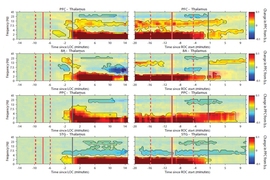
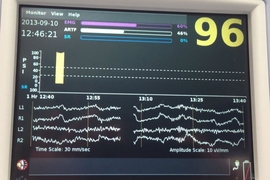
A motivating observation for the pair’s hypothesis is that cardiac arrest patients treated with hypothermia, Covid-19 patients with prolonged wake-ups after sedation and ventilation, and the hibernating painted turtle all exhibit a brain rhythm pattern called “burst suppression.” In the same journal a decade ago, ShiNung Ching, Brown, and co-authors described a model suggesting that burst suppression is an activity pattern signaling that the brain is reducing energy use when sufficient supplies are not available. In this way, the brain limits the damage that neurons could otherwise endure by trying to operate at full power.
“Biophysical modeling has shown that burst suppression is likely a signature of a neurometabolic state that preserves basic cellular function during states of lowered energy availability,” the authors wrote.
The turtles appear to achieve this state by rapidly ramping up the release of GABA, a neurotransmitter chemical known to reduce neural activity in the brain, hours after oxygen becomes scarce. This GABA release, known as the “endogenous anesthesia for the anoxic turtle brain,” reduces the energy demand of brain cells. The authors see a direct parallel in Covid patients who are often given sedatives whose effects are mediated by GABA.
Speeding recovery
If Brown and Schiff’s hypotheses are correct, they write, then there may be a principled two-part approach for better reviving Covid patients from unconsciousness after ventilation is removed.
The first part is to administer Szeto-Schiller peptides (small protein fragments) that are known to improve neurons’ production of the energy metabolism molecule ATP. This could restore the brain cells’ ability to produce energy when they return to a more active state.
The second part calls for a pair of drugs that will restore neural activity and communication by promoting the neurotransmitters glutamate and acetylcholine, essentially counteracting GABA’s tamping down of neural activity and metabolism.
“Our analysis predicts the existence of a human form of PDS that may underlie prolonged recovery of consciousness following treatment for severe Covid-19 or treatment for post-cardiac arrest treated with hypothermia,” Brown and Schiff wrote. “The possible existence of human PDS suggests many testable hypotheses for further investigation and the possibility of developing novel therapeutic strategies.”