Though many people with autism spectrum disorders also experience unusual gastrointestinal inflammation, scientists have not established how those conditions might be linked. Now MIT and Harvard Medical School researchers, working with mouse models, may have found the connection: When a mother experiences an infection during pregnancy and her immune system produces elevated levels of the molecule Interleukin-17a (IL-17a), this can not only alter brain development in her fetus, but also alter her microbiome such that after birth the newborn’s immune system can become primed for future inflammatory attacks.
In four studies beginning in 2016, study co-senior authors Gloria Choi of MIT and Jun Huh of Harvard University traced how elevated IL-17a during pregnancy acts on neural receptors in a specific region of the fetal brain to alter circuit development, leading to autism-like behavioral symptoms in mouse models. Their new research, published Dec. 7 in Immunity, shows how IL-17a can act to also alter the trajectory of immune system development.
“We’ve shown that IL-17a acting on the fetal brain can induce autism-like behavioral phenotypes such as social deficits,” says Choi, the Mark Hyman Jr. Career Development Associate Professor in The Picower Institute for Learning and Memory and Department of Brain and Cognitive Sciences at MIT. “Now we are showing that the same IL-17a in mothers, through changes in the microbiome community, produces co-morbid symptoms such as a primed immune system.”
The researchers caution that the study findings are yet to be confirmed in humans, but that they do offer a hint that central nervous and immune system problems in individuals with autism-spectrum disorders share an environmental driver: maternal infection during pregnancy.
“There has been no mechanistic understanding of why patients with a neurodevelopmental disorder have a dysregulated immune system,” says Huh, an associate professor of immunology at Harvard Medical School. “We’ve tied these fragmented links together. It may be that the reason is that they were exposed to this increase in inflammation during pregnancy.”
Eunha Kim and Donggi Paik of Huh’s lab are the study’s co-lead authors.
Tracking timing
The research team first confirmed that maternal immune activation (MIA) leads to enhanced susceptibility to intestinal inflammation in offspring by injecting pregnant mice with poly(I:C), a substance that mimics viral infection. Their offspring, but not the offspring of mothers in an unaffected control group, exhibited autism-like symptoms, as expected, and also gut inflammation when exposed to other inflammatory stimuli.
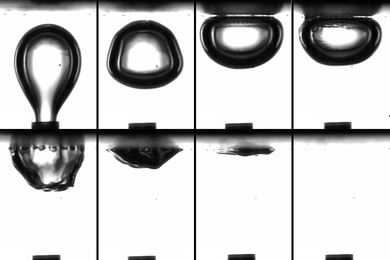
While the neurodevelopmental aberrations the team has tracked occur while the fetus is still in the womb, it was not clear when the altered immune responses developed. To find out, the team switched mouse pups at birth so that ones born to MIA moms were reared by control moms and ones born to control moms were reared by MIA moms. The team found that pups born to MIA moms but reared by control moms exhibited the autism symptoms but not the intestinal inflammation. Pups born to control moms but reared by MIA moms did not show autism symptoms, but did experience intestinal inflammation. The results showed that while neurodevelopment is altered before birth, the immune response is altered postnatally.
Microbiome-mediated molecular mechanism
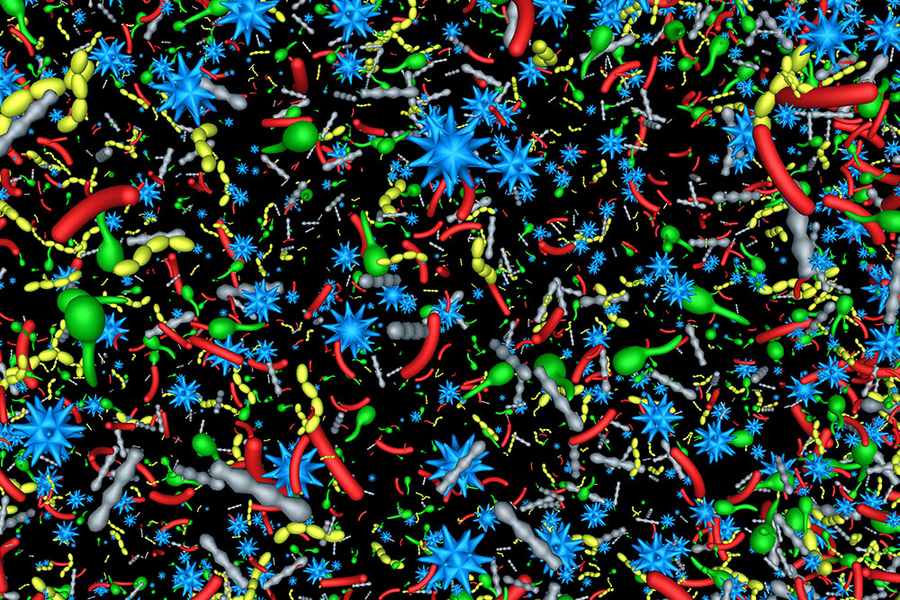
The question then became how MIA moms have this postnatal effect on pups. Other studies have found that the maternal microbiome can influence the immune system development of offspring. To test whether that was the case in the MIA model, the researchers examined stool from MIA and control mice and found that the diversity of the microbial communities were significantly different.
Then, to determine whether these differences played a causal role, they raised a new set of female mice in a “germ-free” environment, meaning that they do not carry any microbes in or on their body. Then the scientists transplanted stool from MIA or control moms into these germ-free moms and bred them with males. Unlike with the controls, pups born to MIA-stool-transferred moms exhibited the intestinal inflammation. These results indicated that the altered microbiome of MIA moms leads to the immune priming of offspring.
Among the notable differences the team measured in the intestinal inflammation response was an increase in IL-17a production by immune system T cells. IL-17a is the same cytokine whose levels are upregulated in MIA moms. When the scientists looked at T cells from MIA-microbiome-exposed offspring versus control offspring they found that in MIA-offspring, CD4 T cells were more likely to differentiate into Th17 cells, which release IL-17a.
That prompted them to look at potential differences in how the CD4 T cells of the different groups transcribe their genes. MIA-microbiome-exposed CD4 T cells exhibited higher expression of genes for T cell activation, suggesting they were more primed for T cell-dependent immune responses in response to infections.
“Thus, increase in IL-17a in moms during pregnancy leads to susceptibility to produce more IL-17a in offspring upon an immune challenge,” Choi says.
Having established that the immune system of offspring can become mis-primed by exposure to the altered microbiome of a mother who was infected during pregnancy, the remaining question was how that microbiome becomes altered in the first place. Suspecting IL-17a, the team tested the effects of antibodies that block the cytokine. When they blocked IL-17a in moms prior to immune activation, their offspring did not exhibit the intestinal inflammation later in life. This also held true when the researchers repeated the experiment of transplanting MIA stool to germ-free moms, this time including stool from MIA-moms with IL-17a blockers. Again, blocking IL-17a amid maternal infection led to a microbiome that did not mis-prime the immune system of offspring.
Long-term questions
Huh said the results highlight that environmental exposures during pregnancy, such as infection, can have long-term health consequences for offspring, a concern that has always been present but that may be exacerbated by the Covid-19 pandemic. Further study is needed, he said, to determine long-term effects on children born to mothers infected with SARS-Cov-2.
Choi added that emerging connections between inflammation and neurodegenerative diseases such as Alzheimer’s may also warrant further study, given the team’s findings of how maternal infection can lead to enhanced inflammation in offspring.
In addition to Choi, Huh, Kim, and Paik, the paper’s other authors are Ricardo Ramirez, Delaney Biggs, Youngjun Park, and Ho-Keun Kwon.
The National Research Foundation of Korea, the Jeongho Kim Neurodevelopmental Research Fund, The Simons Foundation Autism Research Initiative, the National Institutes of Health, the N of One Autism Research Foundation, and the Burroughs Wellcome Fund provided funding for the study.