In Belize, where diabetes is rampant, patients need insulin every day to maintain proper blood sugar levels. But if people lack electricity or a refrigerator, they cannot store insulin at home. Medical advice pamphlets encourage such patients to keep their insulin in the refrigerators at small corner grocery stores instead. And so, in some cases, there the insulin sits — right next to soft drinks which, in good measure, have helped cause the growing diabetes epidemic in the first place.
“That one image, of soda bottles and the insulin side by side, has stuck with me,” says Amy Moran-Thomas, an MIT professor and cultural anthropologist who has spent over 10 years researching and writing about the global diabetes epidemic. “It’s emblematic of the larger problem, a robust infrastructure even in rural areas to deliver foods that are contributing to diabetes, and the huge gaps in global infrastructure for treating the same conditions.”
The International Diabetes Foundation estimates that 425 million people currently have diabetes, and that number is expected to increase to more than 600 million within a generation. (By the foundation’s count, annual diabetes deaths now outnumber those from HIV/AIDS and breast cancer, combined.) U.N. Secretary General Ban Ki-moon has called chronic illnesses such as diabetes a “public health emergency in slow motion.”
Now Moran-Thomas has chronicled that emergency in a new book, “Traveling with Sugar: Chronicles of a Global Epidemic,” published this month by the University of California Press. In it, Moran-Thomas examines the havoc diabetes has caused in Belize, a Central American country with resource limitations — annual per capita income is under $5,000 — and one that is heavily reliant on cheap, high-glucose foods made with white rice, white flour, and white sugar.
“Before I started getting to know people, I had this idea that infectious diseases were the primary health crisis in a lot of Central America,” says Moran-Thomas, who as a graduate student initially considered studying the problems of parasitic infections. Instead, she discovered, “Everyone was talking about diabetes.”
Looking at the scope of the problem as well as its causes, Moran-Thomas says she came to regard the situation in Belize as a case study in how lives are rearranged by the spread of diabetes globally: “I felt this was part of something bigger that was happening in the world.”
Vanishing from the photo album
Diabetes is a disease with many possible consequences. Patients often feel excessively thirsty or hungry, although those are just early symptoms; complications and effects over time can lead to heart failure, stroke, kidney failure, blindness, and amputation of limbs, among other things. Diabetes is so strongly associated with managing blood sugar levels that the word “sugar” has become a virtual synonym for the illness in many places; in Belize “traveling with sugar” is a common expression for living with diabetes.
Moran-Thomas conducted her ethnographic research in collaboration with people in Belize, getting to know many families and community caregivers. She also conducted years of archival research about the social context, reconstructing the history of colonialism and commerce that has left Belize largely impoverished and dependent on outside sources for food and income.
Grappling with matters that resonate across the Caribbean, Latin America, and beyond, “Traveling with Sugar” closely examines how sugar-heavy diets became so common. This includes issues such as the legacy of plantation landscapes on contemporary agriculture, and the ways diabetes risks are compounded by toxic pollution, climate change, stressful social environments, and interruptions of therapy.
The human consequences are stark. Among the stories Moran-Thomas chronicles in the book, one involves an older man lovingly paging through a family photo album showing how his late wife, a teacher, had endured multiple amputations — first a foot, then both legs below the knees — which became woven into the family’s larger story of caring for each other. In the family photo album, Moran-Thomas writes, “we watched her disappear a piece at a time from the pictures, until she was absent altogether.”
As people’s bodies have changed, Moran-Thomas observes, the local landscape has too. The first place where she conducted an interview in Belize is now under water, due to coastal erosion and sea-level rise. Such cases will become more common in Belize and around the world, Moran-Thomas thinks, if the global economy promoting the growth of “carbohydrates and hydrocarbons” continues unaltered.
“There is so much profit being made from the products that contribute to the condition, and there is also money to be made for treating its harmful effects,” she notes. “So it’s difficult to think about interrupting this engine, when money’s being made on both sides, of causing and treating a problem.”
Belize’s status as a resort area also leads to some incongruous scenes in the book. Oxygen-rich hyperbaric chambers can help prevent diabetic amputations, and do exist in Belize — but primarily for tourists, such as divers with the bends. Many Belizean citizens have barely heard of such devices, let alone used them for diabetes care.
“There is a segregation of infrastructures,” Moran-Thomas says. “The hyperbaric chambers exemplify that — Caribbean residents dying from amputations without being able to access the chambers in their own countries.”
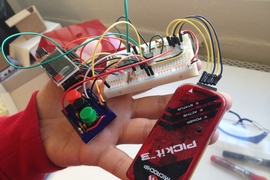
Grassroots initiatives and equitable design
The research behind “Traveling with Sugar” has already been the basis of interdisciplinary work at MIT, where Moran-Thomas has collaborated with Jose Gomez-Marquez and other members of the Little Devices Lab to create a new MIT course, 21A.311 (Social Lives of Medical Objects). One focal point of the class involves bringing together readings with lab exercises to examine what the sociologist Ruha Benjamin has called “discriminatory design” — the outcome of which is that objects and devices can be impossible for many people to use effectively.
“Discrimination doesn’t have to be intentional in order to produce a pattern of exclusion that really impacts people,” Moran-Thomas says.
For instance, she adds, “Glucose meters can’t really be repaired by the people who need them most to thrive. This makes life so much harder for people who need those meters to safely manage drugs like insulin. I think that’s an additional entry point for thinking about the delivery of health care — the assumptions built into objects has a huge impact on delivery working. At places like MIT, co-created design ideas can be put into practice. [The students] did some amazing final projects for that class, trying to reimagine what equitable objects could look like.”
Beyond medical technologies, and alongside large-scale national or international action, Moran-Thomas suggests, the ongoing work many communities are doing to reverse the diabetes epidemic from the ground up deserves more recognition and resources.
“The grassroots level is where I saw the most committed work for real change,” says Moran-Thomas, citing projects like a diabetic foot care group working to prevent amputations and a local farming cooperative building a healthy-cereal program.
“I don’t know how to reorganize a global trade system — though more policies trying to address those things are absolutely crucial,” she adds. “But there are so many tiny, vital steps that people are already working on at the level of their own neighborhoods and communities. I focused on those stories in the book to show how a future approach to diabetes response can build from that grassroots scale.”