With the recent launch of MIT’s Institute for Medical Engineering and Science, MIT News examines research with the potential to reshape medicine and health care through new scientific knowledge, novel treatments and products, better management of medical data, and improvements in health-care delivery.
When clinicians in a Boston-area hospital wish there was a device that could meet some specific need, they have a chance to do something about it: They can add it to a wish list to be presented each fall to a class of mechanical engineering students at MIT. These budding engineers then spend a semester coming up with ideas, and eventually prototypes, to solve selected problems.
Sometimes these projects, from a class called Precision Machine Design — known as 2.75 in MIT’s class-numbering system (or 2.750 for undergraduates) — actually end up becoming real products.
Physicians who perceive a need for a new device can submit a two-page proposal detailing the desired functionality and requirements. About 30 such requests are submitted each year; the class instructors whittle the number to about a dozen, selecting those that are challenging, yet of a scope that can realistically be tackled by students in a semester of designing and prototyping. Students, however, make the ultimate selection.
Another important criterion is that the doctors have to be interested enough to work closely with the students throughout the process. “We want physicians who are engaged and accessible,” says Nevan Hanumara, a former student in the class who now co-teaches it as an MIT postdoc.
“They need to be prepared to meet with them at least once every two weeks,” he says, noting that each student should expect to “call your clinician by their first name.”
It’s crucial that all members of the team, be they physicians or undergraduates, feel like equals in the process of developing the new tool, Hanumara adds.
The class, which assumed its medical-devices emphasis in 2004, was a co-creation of MIT professor Alexander Slocum and an organization of Boston-based doctors called the Center for Integration of Medicine and Innovative Technology, or CIMIT.
In a related earlier course, students came up with concepts and business plans for such devices, but didn’t actually build working versions to test the ideas, says Slocum, the Neil and Jane Pappalardo Professor of Mechanical Engineering. But when it’s all just designs on paper, he says, “It’s too easy to gloss over details. I was excited by the projects, but disappointed by the amount of detail.”
So Slocum decided to evolve the class into its present project-based form. He continues to teach the class, along with Hanumara, three teaching assistants, and Charles Sodini, the Clarence J. LeBel Professor of Electrical Engineering, who is helping to reinforce the increasing importance of electronics in medical devices. In fact, starting in the fall 2014 semester, it will become a joint course with the Department of Electrical Engineering and Computer Science and be renamed “Medical Device Design.”
Sodini says that the idea behind the change is that "Electronics adds the 'smarts' to these devices to acquire, store, and process data, as well as improve the user interface for easier operation by the clinicians."
It’s not enough to come up with good ideas, Slocum says. “There’s an underlying principle of precision,” he says. “Anything mechanical has to have some level of precision to it” — making this exercise a useful one even for students who go on to work in some other area of mechanical engineering.
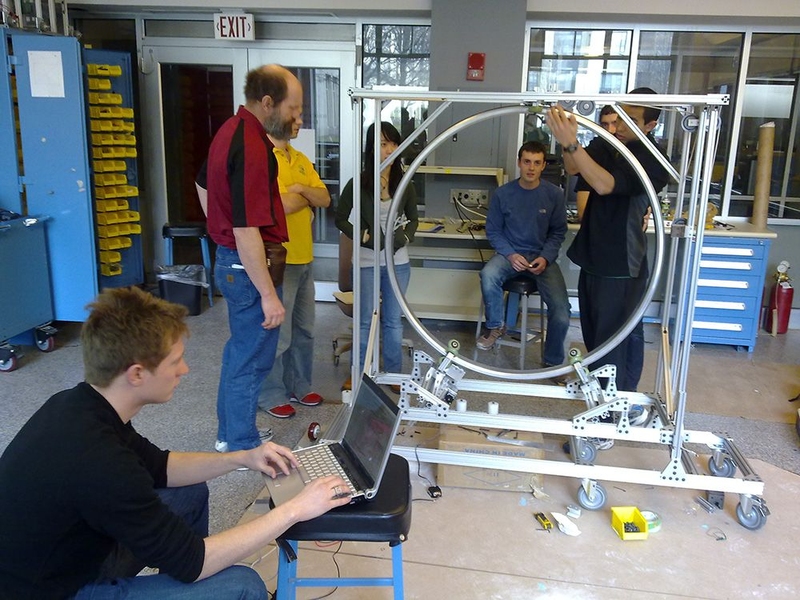
At the beginning of the semester, the doctors come to the class and present their ideas of what they need; the roughly 50 students select projects that interest them. By the end of the semester, each team of about four students will have brainstormed, selected a concept to focus on, and built a working proof-of-concept of the proposed solution.
For example: Doctors wondered if there might be a simpler and less-invasive way of assessing patients with sleep problems, who must now spend a night in a hospital or clinic wearing dozens of electrodes connected to expensive electronic equipment. In response, a team of students came up with a “sleep sensing shirt” that patients could wear at home, in their own beds. The shirt could record enough data about breathing patterns to provide answers at a fraction of the cost — and inconvenience — of the standard approach.
That concept is now undergoing extensive testing, Hanumara says, on its way to commercialization by a Boston-based company, called Rest Devices, that former students and their medical mentor have set up.
Other projects that grew out of the class and are now en route to commercialization include an endoscopic screwdriver, to be used for repairing broken ribs without open-chest surgery, and a low-cost device to apply negative pressure to wounds in order to speed healing.
Students, realizing that they are working on potential solutions to serious problems, tend to throw themselves into the projects with great enthusiasm and dedication, Hanumara says. Even over the Thanksgiving holiday, he received messages from students asking for approval to order parts for their devices. (Each team is given a budget of $4,000, thanks to CIMIT and corporate sponsors.)
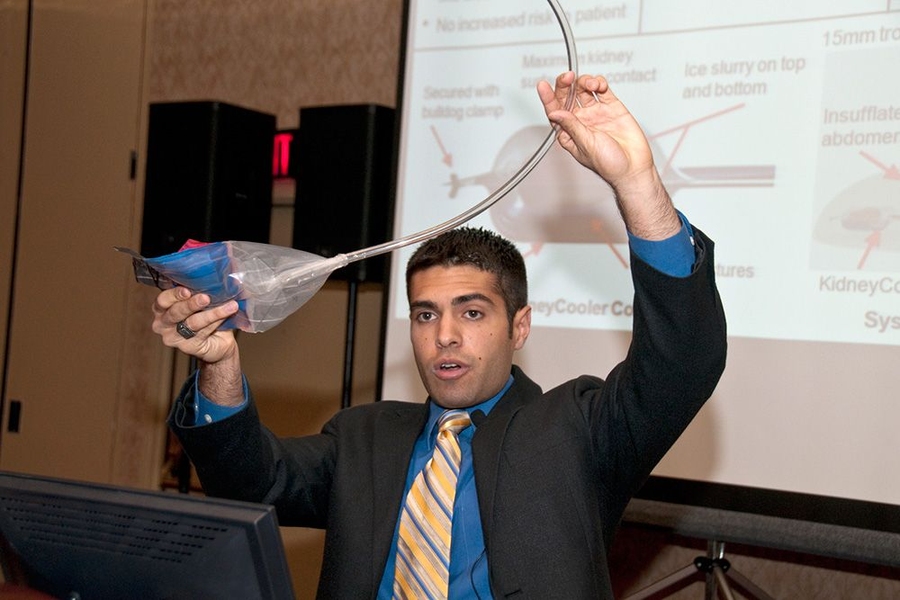
By the end of the class, students not only develop working devices, but also become familiar with budgeting and business plans and gain skill in explaining their ideas succinctly and clearly. Many go on to present their work at the annual Design of Medical Devices conference or other professional meetings in the field. Those who wish to continue can do so in a spring-semester follow-up, 2.753 (Development of Mechanical Products). Most importantly, data indicates that students are taking the class with the goal of landing jobs in the medical device design industry and succeeding in this aim. Some are even offering to come back to the class as speakers and recruiters.
“Two-thirds of the students go on,” Hanumara says, to take their ideas from a proof-of-concept to an actual prototype. About three-quarters of those who take the two courses are graduate students, though both are open to MIT seniors as well.
The class is unusual — both at MIT and in industry — in its rapid accomplishment of the entire product-design cycle. “Companies come to us,” Hanumara says, because “our innovation process is quicker than theirs.” But despite the speed, every step of a product’s development and testing has to be carefully documented to ensure the results are valid and can be replicated. “If it does work, you have to have the records,” he says.
Many of the class projects produce tangible results. Dozens have resulted in peer-reviewed papers or conference presentations, about a dozen have been patented (or are in the process), and several have been licensed to existing companies or have become the basis of new startups.
“Lots of schools do hands-on, design-build-deliver classes,” Slocum says. But to the best of his knowledge, none of these include such close interaction with the ultimate customers — in this case, doctors and clinicians — who roll up their sleeves and participate as team mentors and members. “Our model is real,” he says.
“Things get better and better every year,” Slocum adds. “More and more projects are ready to become products.”
When clinicians in a Boston-area hospital wish there was a device that could meet some specific need, they have a chance to do something about it: They can add it to a wish list to be presented each fall to a class of mechanical engineering students at MIT. These budding engineers then spend a semester coming up with ideas, and eventually prototypes, to solve selected problems.
Sometimes these projects, from a class called Precision Machine Design — known as 2.75 in MIT’s class-numbering system (or 2.750 for undergraduates) — actually end up becoming real products.
Physicians who perceive a need for a new device can submit a two-page proposal detailing the desired functionality and requirements. About 30 such requests are submitted each year; the class instructors whittle the number to about a dozen, selecting those that are challenging, yet of a scope that can realistically be tackled by students in a semester of designing and prototyping. Students, however, make the ultimate selection.
Another important criterion is that the doctors have to be interested enough to work closely with the students throughout the process. “We want physicians who are engaged and accessible,” says Nevan Hanumara, a former student in the class who now co-teaches it as an MIT postdoc.
“They need to be prepared to meet with them at least once every two weeks,” he says, noting that each student should expect to “call your clinician by their first name.”
It’s crucial that all members of the team, be they physicians or undergraduates, feel like equals in the process of developing the new tool, Hanumara adds.
The class, which assumed its medical-devices emphasis in 2004, was a co-creation of MIT professor Alexander Slocum and an organization of Boston-based doctors called the Center for Integration of Medicine and Innovative Technology, or CIMIT.
In a related earlier course, students came up with concepts and business plans for such devices, but didn’t actually build working versions to test the ideas, says Slocum, the Neil and Jane Pappalardo Professor of Mechanical Engineering. But when it’s all just designs on paper, he says, “It’s too easy to gloss over details. I was excited by the projects, but disappointed by the amount of detail.”
So Slocum decided to evolve the class into its present project-based form. He continues to teach the class, along with Hanumara, three teaching assistants, and Charles Sodini, the Clarence J. LeBel Professor of Electrical Engineering, who is helping to reinforce the increasing importance of electronics in medical devices. In fact, starting in the fall 2014 semester, it will become a joint course with the Department of Electrical Engineering and Computer Science and be renamed “Medical Device Design.”
Sodini says that the idea behind the change is that "Electronics adds the 'smarts' to these devices to acquire, store, and process data, as well as improve the user interface for easier operation by the clinicians."
It’s not enough to come up with good ideas, Slocum says. “There’s an underlying principle of precision,” he says. “Anything mechanical has to have some level of precision to it” — making this exercise a useful one even for students who go on to work in some other area of mechanical engineering.
At the beginning of the semester, the doctors come to the class and present their ideas of what they need; the roughly 50 students select projects that interest them. By the end of the semester, each team of about four students will have brainstormed, selected a concept to focus on, and built a working proof-of-concept of the proposed solution.
For example: Doctors wondered if there might be a simpler and less-invasive way of assessing patients with sleep problems, who must now spend a night in a hospital or clinic wearing dozens of electrodes connected to expensive electronic equipment. In response, a team of students came up with a “sleep sensing shirt” that patients could wear at home, in their own beds. The shirt could record enough data about breathing patterns to provide answers at a fraction of the cost — and inconvenience — of the standard approach.
That concept is now undergoing extensive testing, Hanumara says, on its way to commercialization by a Boston-based company, called Rest Devices, that former students and their medical mentor have set up.
Other projects that grew out of the class and are now en route to commercialization include an endoscopic screwdriver, to be used for repairing broken ribs without open-chest surgery, and a low-cost device to apply negative pressure to wounds in order to speed healing.
Students, realizing that they are working on potential solutions to serious problems, tend to throw themselves into the projects with great enthusiasm and dedication, Hanumara says. Even over the Thanksgiving holiday, he received messages from students asking for approval to order parts for their devices. (Each team is given a budget of $4,000, thanks to CIMIT and corporate sponsors.)
By the end of the class, students not only develop working devices, but also become familiar with budgeting and business plans and gain skill in explaining their ideas succinctly and clearly. Many go on to present their work at the annual Design of Medical Devices conference or other professional meetings in the field. Those who wish to continue can do so in a spring-semester follow-up, 2.753 (Development of Mechanical Products). Most importantly, data indicates that students are taking the class with the goal of landing jobs in the medical device design industry and succeeding in this aim. Some are even offering to come back to the class as speakers and recruiters.
“Two-thirds of the students go on,” Hanumara says, to take their ideas from a proof-of-concept to an actual prototype. About three-quarters of those who take the two courses are graduate students, though both are open to MIT seniors as well.
The class is unusual — both at MIT and in industry — in its rapid accomplishment of the entire product-design cycle. “Companies come to us,” Hanumara says, because “our innovation process is quicker than theirs.” But despite the speed, every step of a product’s development and testing has to be carefully documented to ensure the results are valid and can be replicated. “If it does work, you have to have the records,” he says.
Many of the class projects produce tangible results. Dozens have resulted in peer-reviewed papers or conference presentations, about a dozen have been patented (or are in the process), and several have been licensed to existing companies or have become the basis of new startups.
“Lots of schools do hands-on, design-build-deliver classes,” Slocum says. But to the best of his knowledge, none of these include such close interaction with the ultimate customers — in this case, doctors and clinicians — who roll up their sleeves and participate as team mentors and members. “Our model is real,” he says.
“Things get better and better every year,” Slocum adds. “More and more projects are ready to become products.”