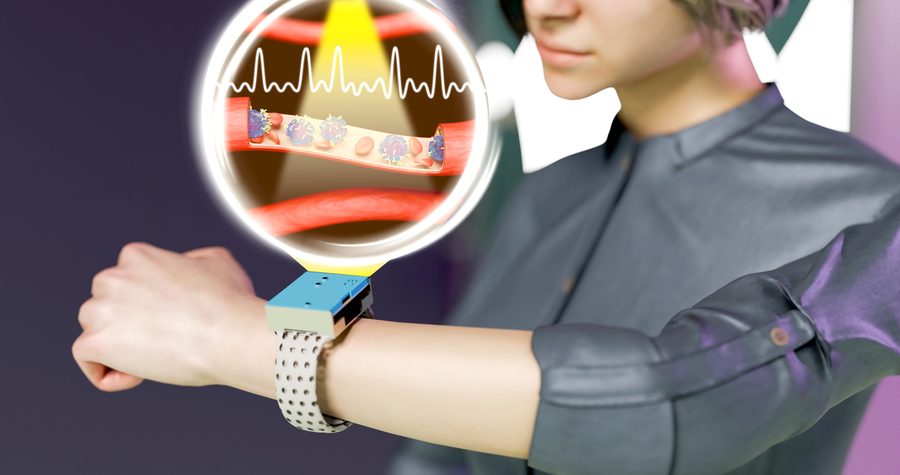
Researchers at MIT have developed a noninvasive medical monitoring device powerful enough to detect single cells within blood vessels, yet small enough to wear like a wristwatch. One important aspect of this wearable device is that it can enable continuous monitoring of circulating cells in the human body.
The technology was presented online on March 3 by the journal npj Biosensing and is forthcoming in the journal’s print version.
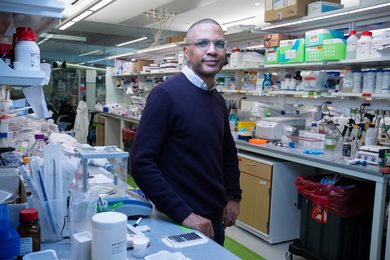
The device — named CircTrek — was developed by researchers in the Nano-Cybernetic Biotrek research group, led by Deblina Sarkar, assistant professor at MIT and AT&T Career Development Chair at the MIT Media Lab. This technology could greatly facilitate early diagnosis of disease, detection of disease relapse, assessment of infection risk, and determination of whether a disease treatment is working, among other medical processes.
Whereas traditional blood tests are like a snapshot of a patient’s condition, CircTrek was designed to present real-time assessment, referred to in the npj Biosensing paper as having been “an unmet goal to date.” A different technology that offers monitoring of cells in the bloodstream with some continuity, in vivo flow cytometry, “requires a room-sized microscope, and patients need to be there for a long time,” says Kyuho Jang, a PhD student in Sarkar’s lab.
CircTrek, on the other hand, which is equipped with an onboard Wi-Fi module, could even monitor a patient’s circulating cells at home and send that information to the patient’s doctor or care team.
“CircTrek offers a path to harnessing previously inaccessible information, enabling timely treatments, and supporting accurate clinical decisions with real-time data,” says Sarkar. “Existing technologies provide monitoring that is not continuous, which can lead to missing critical treatment windows. We overcome this challenge with CircTrek.”
The device works by directing a focused laser beam to stimulate cells beneath the skin that have been fluorescently labeled. Such labeling can be accomplished with a number of methods, including applying antibody-based fluorescent dyes to the cells of interest or genetically modifying such cells so that they express fluorescent proteins.
For example, a patient receiving CAR T cell therapy, in which immune cells are collected and modified in a lab to fight cancer (or, experimentally, to combat HIV or Covid-19), could have those cells labeled at the same time with fluorescent dyes or genetic modification so the cells express fluorescent proteins. Importantly, cells of interest can also be labeled with in vivo labeling methods approved in humans. Once the cells are labeled and circulating in the bloodstream, CircTrek is designed to apply laser pulses to enhance and detect the cells’ fluorescent signal while an arrangement of filters minimizes low-frequency noise such as heartbeats.
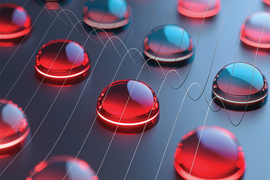
“We optimized the optomechanical parts to reduce noise significantly and only capture the signal from the fluorescent cells,” says Jang.
Detecting the labeled CAR T cells, CircTrek could assess whether the cell therapy treatment is working. As an example, persistence of the CAR T cells in the blood after treatment is associated with better outcomes in patients with B-cell lymphoma.
To keep CircTrek small and wearable, the researchers were able to miniaturize the components of the device, such as the circuit that drives the high-intensity laser source and keeps the power level of the laser stable to avoid false readings.
The sensor that detects the fluorescent signals of the labeled cells is also minute, and yet it is capable of detecting a quantity of light equivalent to a single photon, Jang says.
The device’s subcircuits, including the laser driver and the noise filters, were custom-designed to fit on a circuit board measuring just 42 mm by 35 mm, allowing CircTrek to be approximately the same size as a smartwatch.
CircTrek was tested on an in vitro configuration that simulated blood flow beneath human skin, and its single-cell detection capabilities were verified through manual counting with a high-resolution confocal microscope. For the in vitro testing, a fluorescent dye called Cyanine5.5 was employed. That particular dye was selected because it reaches peak activation at wavelengths within skin tissue’s optical window, or the range of wavelengths that can penetrate the skin with minimal scattering.
The safety of the device, particularly the temperature increase on experimental skin tissue caused by the laser, was also investigated. An increase of 1.51 degrees Celsius at the skin surface was determined to be well below heating that would damage tissue, with enough of a margin that even increasing the device’s area of detection, and its power, in order to ensure the observation of at least one blood vessel could be safely permitted.
While clinical translation of CircTrek will require further steps, Jang says its parameters can be modified to broaden its potential, so that doctors could be provided with critical information on nearly any patient.