“Not that many years ago, if you had a blocked coronary artery, you would be asked to tough it out, or have open-heart surgery,” says Elazer Edelman, the Thomas D. and Virginia W. Cabot Professor of Health Sciences and Technology at MIT. “Both involved significant suffering and there was nothing to provide in between.”
“Today, we can relieve that obstruction within a matter of minutes with an endovascular stent, a metal-mesh tube that can be threaded up from an artery in an arm or a leg,” adds Edelman, a cardiovascular physician and bioengineer who directs both the Harvard-MIT Biomedical Engineering Center and the MIT Clinical Research Center.
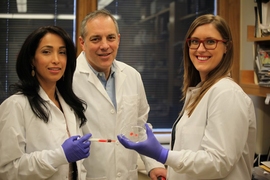
Edelman and his students helped develop the first stents and successive generations of these devices, including versions that are coated to release drugs to prevent cells from building up around the stent and blocking it. “We worked with the best scientists in academia and industry to understand how to most effectively create a combination product,” he says. “Now millions of people around the world every year get one of these devices, and virtually all of the clinically available products are based on work in our MIT laboratories.”
Edelman, who is also a professor of medicine at Harvard Medical School, leads multidisciplinary teams that bring innovation to cardiovascular care. “Our research leverages basic findings in biology, applied physiology, engineering and other sciences to rapidly translate ideas from conceptiond to clinical introduction,” he says. “That requires a fluency in multiple disciplines but also working with scientists in industry.”
Fixes in the blood
Although it once was thought that diseases of the heart and the blood vessels were important only in affluent countries, these illnesses affect every nation around the world, Edelman emphasizes. Until now, only higher-income countries have enjoyed access to innovative treatment technologies.
“However, innovation in medicine carries an obligation and a challenge — the need to ensure that all gain use of these creations,” he says. “We’ve realized that part of the creativity is in providing access, and that simple solutions to complex problems can often enable broad appeal and use.”
Endovascular stents offer one example of such solutions, he points out. Another comes from his group’s work on heart valves that can be placed minimally invasively.
More and more people live long enough to have problems with their heart valves, and until recently the surgery was so intrusive that only those with no alternative have received the operation, Edelman explains. He and his colleagues are studying ways to replace valves by inserting a catheter, as is done with endovascular stents. They work both to optimize the technology and to make sure that it’s available to as many people who can benefit as possible.
Another major effort focuses on mechanical means of reducing high blood pressure, which is a major silent killer. Edelman marshaled his lab’s resources to examine the emerging field of “renal denervation” — a technology that holds great promise for people with high blood pressure that doesn’t respond well to drugs but has stumbled in clinical studies.
In renal denervation, devices inserted by catheter can deliver carefully aimed radio frequency emissions to burn out the nerves on kidney arteries, and in doing so reduce blood pressure. Early clinical studies were promising, but a recent large international trial showed no significant effect.
Edelman and his group, however, managed to explain the disparate findings and rejuvenate the field. By combining pre-clinical and clinical analyses with insightful computational analyses, they created a comprehensive model for understanding renal denervation. The model demonstrates that the technique can work, but its effectiveness depends on the extent of nerve destruction, which in turn is determined by the local tissue anatomy around the device’s energy-emitting electrodes.
These themes of innovation and access apply to the lab’s work on biological constructs, as well as mechanical devices, Edelman says.
“We worked for years on the basic biology of the cell that lines blood vessels, the endothelial cell,” he says. His lab and other groups demonstrated that the health of a blood vessel was directly related to the health of its lining — and that if the lining was diseased or otherwise disabled, introducing healthy endothelial cells could restore blood vessel health.
Bringing these cells into therapy was the next step, and doing so required a mastery not just of cell biology but cell engineering, he emphasizes. “We created material constructs that could house the cells, transport the cells, allow them to remain viable on a shelf from months to years, and allow them to be placed in confined spaces while still retaining all of their biology,” he says. “This form of cell engineering required sophistication in material science but also in cell and molecular biology.”
After many years of development, the tissue engineering technique is being tested in five clinical trials of patients with arterial disease.
Learning the languages
Solving such puzzles, and moving such innovative treatments into the clinic, requires a broad collection of expertise — and that is not easily brought to bear.
“The challenge and the opportunity in multidisciplinary science is to allow all the disciplines to grow but not grow apart,” Edelman remarks.
Rapid progress in diagnosing and treating major diseases “require that we train people differently, and we train people to think about what we do differently,” he says. “We need to make everyone in the room not only recognize that there’s another language but understand those other languages. We need to train engineers so they not only appreciate biology but know biology. We need biologists who understand mathematics, mathematicians who understand material sciences, and on and on.”
Importantly, realizing the benefits of research also depends entirely on industrial collaboration. “Students get to work hand-in-hand with industry on the realization of the endless potential of new ideas,” Edelman says. “And they increasingly choose to go to industry, because they know that industrial partners have resources that even we at MIT don’t have. MIT in turn can provide assets that industry doesn’t have — this constant source of brilliant young minds. MIT can bring in ideas from many disciplines to create these hybrid combination products that are increasingly becoming the transformative technologies of the next decade.”
“It’s a really exciting time to be a biomedical engineer and a translational scientist,” he adds. “The pace of discovery is rapid and the pace of commercialization keeps track, allowing our ideas to move from concept to clinic rapidly and safely.”