When people become infected by HIV, it’s usually only a matter of time, barring drug intervention, until they develop full-blown AIDS. However, a small number of people exposed to the virus progress very slowly to AIDS — and some never develop the disease at all.
In the late 1990s, researchers showed that a very high percentage of those naturally HIV-immune people, who represent about one in 200 infected individuals, carry a gene called HLA B57. Now a team of researchers from the Ragon Institute of Massachusetts General Hospital, MIT and Harvard has revealed a new effect that contributes to this gene’s ability to confer immunity.
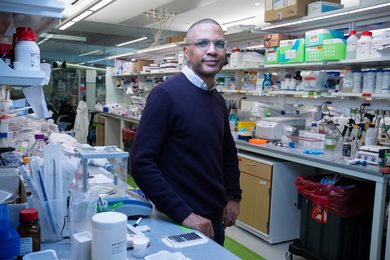
The research team, led by MIT Professor Arup Chakraborty and Harvard Professor Bruce Walker of MGH, found that the HLA B57 gene causes the body to make more potent killer T cells — white blood cells that help defend the body from infectious invaders. Patients with the gene have a larger number of T cells that bind strongly to more pieces of HIV protein than people who do not have the gene. This makes the T cells more likely to recognize cells that express HIV proteins, including mutated versions that arise during infection. This effect contributes to superior control of HIV infection (and any other virus that evolves rapidly), but it also makes those people more susceptible to autoimmune diseases, in which T cells attack the body’s own cells.
This new knowledge, described in the May 5 online edition of Nature, could help researchers develop vaccines that provoke the same response to HIV that individuals with HLA B57 muster on their own, says Walker, who is director of the Ragon Institute and a professor at Harvard Medical School.
“HIV is slowly revealing itself,” says Walker. “This is another point in our favor in the fight against the virus, but we have a long way to go.”
Natural resistance
Chakraborty, a professor of chemical engineering, chemistry and biological engineering who specializes in theoretical and computational studies of the immune system, undertook this study after Walker told him about the phenomenon of HLA B57-induced immunity. Chakraborty was also intrigued by the fact that people who carry the HLA B57 gene also are more likely to develop autoimmune disorders.
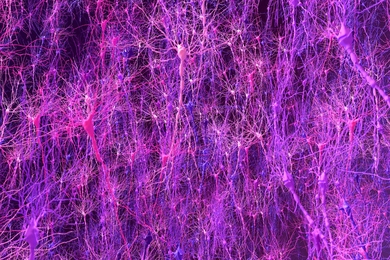
Chakraborty, Walker and their colleagues focused on killer T cells, one of two types of T cells that play an important role in the immune response. Most killer T cells are genetically unique and recognize different pieces of foreign proteins, known as epitopes, attached to the surface of cells that have been infected by viruses or bacteria.
After a killer T cell grabs hold of such a protein, it becomes activated and starts sweeping the body for more cells that express the same protein, so it can kill them. It also clones itself to produce an army of T cells targeting the invader.
The new Ragon Institute study shows that individuals with the HLA B57 gene produce larger numbers of killer T cells that are cross-reactive, meaning they can attack more than one epitope associated with HIV, including mutants that arise to escape activated killer T cells.
The finding offers hope that researchers could design a vaccine to help draw out cross-reactive T cells in people who don’t have the HLA B57 gene. “It’s not that they don’t have cross-reactive T cells,” says Chakraborty. “They do have them, but they’re much rarer, and we think they might be coaxed into action with the right vaccine.”
The work is a valuable contribution to scientists’ understanding of HIV, says David Baltimore, professor of biology and former president of Caltech.
“This is a remarkable paper because it starts from a clinical observation, integrates it with experimental observations, generates a valuable model and derives from the model a deep understanding of the behavior of the human immune system. Rarely does one read a paper that stretches the mind so surprisingly far,” says Baltimore, a Nobel laureate in physiology or medicine who now studies HIV and human T cell interactions.
Weeding out
Chakraborty and colleagues had previously developed computational models of T-cell development in the thymus, an organ located behind the breastbone through which T cells must pass in order to become mature killers. There they undergo a selection process designed to weed out cells that might attack the body’s own cells (which display pieces of human proteins on their surface). T cells must also demonstrate that they can bind weakly to some human protein fragments. Only a tiny percentage of T cells pass these tests and are allowed to leave the thymus and circulate in the body to defend against viruses, other diseases, and cancerous cells.
Inside the thymus, T cells are exposed to “self-peptides” — small human protein fragments — bound to HLA proteins. Chakraborty and co-workers had previously shown that the diversity of self-peptide fragments presented in the thymus influences the kinds of T cells a person can produce. The type and number of self-peptides expressed are determined by the HLA genes, which have hundreds of distinct forms, including HLA B57. Each person carries up to six of them (three inherited from each parent).
Using data from previous studies, the Ragon team found that HLA B57 protein presents fewer types of self-peptides than most other HLA proteins. (HLA B27 is another protein that presents few types of self-peptides and also appears to protect against HIV and promote autoimmune disorders.) In this study, Chakraborty and postdoctoral fellow Elizabeth Read and graduate student Andrej Kosmrlj, lead authors of the paper, used their computer model to study what happens when maturing T cells are exposed to only a small diversity of self-peptides in the thymus.
T cells with receptors that bind strongly to any of the self-peptides in the thymus are forced to undergo cell suicide, because of their potential to attack the body’s own cells. Chakraborty and co-workers showed that this means that, for most individuals, most of the body’s T cells have receptors that bind to targeted viral proteins via a number of weak interactions, with each interaction making a significant contribution to the binding. Thus, a single mutation to an HIV peptide can potentially evade the immune response.
A different scenario unfolds in people who have the HLA B57 gene. Using their computer model, Chakraborty and colleagues showed that, because those individuals’ T cells are exposed to fewer self-peptides in the thymus, T cells with receptors that mediate strong binding to viral proteins via just a few important contacts are more likely to escape the thymus. This makes these T cells more cross-reactive to targeted HIV peptide mutants, because as long as those points in the viral proteins don’t mutate, the T cells are still effective. The model also showed that once those T cells are released into the bloodstream, they can effectively attack HIV proteins, even when the virus mutates.
This model also explains why people with the HLA B57 gene have autoimmune problems: Their T cells are more likely to bind strongly to human peptides not encountered in the thymus.
The computational studies explained many puzzles, but also made a prediction: Individuals with HLA genes that result in a display of fewer self-peptides should control HIV (and other viruses like hepatitis C virus) better. To test this prediction, the researchers studied nearly 2,000 patients — 1,100 “HIV controllers” and 800 who progressed normally to AIDS, and confirmed that this appears to be true.
‘A horrific global problem’
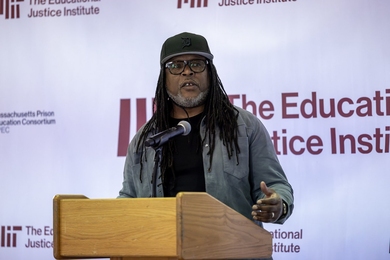
The melding of complementary approaches — clinical studies, basic immunology and computations rooted in engineering and the physical sciences — exemplified by this study is part of the mission of the Ragon Institute, founded last year to support discovery of an effective AIDS vaccine.
The idea is to break down the “scientific silos” in which many researchers work, says Walker. “Because of the Ragon funding, Arup and I had a conversation we never would have otherwise had,” he says. “We probably never would have met.”
There are now a few dozen researchers working on Ragon-funded HIV studies, and Walker believes those new collaborations can lead to many more successes. “There are people out there who have never worked on HIV problems that have something to immediately contribute, and this is a great example of that,” he says. “We have not yet brought the full potential of scientific knowledge to bear on trying to do something about HIV, which remains a horrific global problem.”
The research was also partly funded by Chakraborty’s NIH Director’s Pioneer Award. “Combining fundamental understanding of molecular mechanisms underlying immune function with computational methods for scanning large numbers of sequences allowed the development of a powerful explanation for a problem of great importance to public health. Such interdisciplinary research results are one of the goals of the NIH Director’s Pioneer Award program,” says Jeremy M. Berg, director of the National Institute of General Medical Sciences.
In the late 1990s, researchers showed that a very high percentage of those naturally HIV-immune people, who represent about one in 200 infected individuals, carry a gene called HLA B57. Now a team of researchers from the Ragon Institute of Massachusetts General Hospital, MIT and Harvard has revealed a new effect that contributes to this gene’s ability to confer immunity.
The research team, led by MIT Professor Arup Chakraborty and Harvard Professor Bruce Walker of MGH, found that the HLA B57 gene causes the body to make more potent killer T cells — white blood cells that help defend the body from infectious invaders. Patients with the gene have a larger number of T cells that bind strongly to more pieces of HIV protein than people who do not have the gene. This makes the T cells more likely to recognize cells that express HIV proteins, including mutated versions that arise during infection. This effect contributes to superior control of HIV infection (and any other virus that evolves rapidly), but it also makes those people more susceptible to autoimmune diseases, in which T cells attack the body’s own cells.
This new knowledge, described in the May 5 online edition of Nature, could help researchers develop vaccines that provoke the same response to HIV that individuals with HLA B57 muster on their own, says Walker, who is director of the Ragon Institute and a professor at Harvard Medical School.
“HIV is slowly revealing itself,” says Walker. “This is another point in our favor in the fight against the virus, but we have a long way to go.”
Natural resistance
Chakraborty, a professor of chemical engineering, chemistry and biological engineering who specializes in theoretical and computational studies of the immune system, undertook this study after Walker told him about the phenomenon of HLA B57-induced immunity. Chakraborty was also intrigued by the fact that people who carry the HLA B57 gene also are more likely to develop autoimmune disorders.
Chakraborty, Walker and their colleagues focused on killer T cells, one of two types of T cells that play an important role in the immune response. Most killer T cells are genetically unique and recognize different pieces of foreign proteins, known as epitopes, attached to the surface of cells that have been infected by viruses or bacteria.
After a killer T cell grabs hold of such a protein, it becomes activated and starts sweeping the body for more cells that express the same protein, so it can kill them. It also clones itself to produce an army of T cells targeting the invader.
The new Ragon Institute study shows that individuals with the HLA B57 gene produce larger numbers of killer T cells that are cross-reactive, meaning they can attack more than one epitope associated with HIV, including mutants that arise to escape activated killer T cells.
The finding offers hope that researchers could design a vaccine to help draw out cross-reactive T cells in people who don’t have the HLA B57 gene. “It’s not that they don’t have cross-reactive T cells,” says Chakraborty. “They do have them, but they’re much rarer, and we think they might be coaxed into action with the right vaccine.”
The work is a valuable contribution to scientists’ understanding of HIV, says David Baltimore, professor of biology and former president of Caltech.
“This is a remarkable paper because it starts from a clinical observation, integrates it with experimental observations, generates a valuable model and derives from the model a deep understanding of the behavior of the human immune system. Rarely does one read a paper that stretches the mind so surprisingly far,” says Baltimore, a Nobel laureate in physiology or medicine who now studies HIV and human T cell interactions.
Weeding out
Chakraborty and colleagues had previously developed computational models of T-cell development in the thymus, an organ located behind the breastbone through which T cells must pass in order to become mature killers. There they undergo a selection process designed to weed out cells that might attack the body’s own cells (which display pieces of human proteins on their surface). T cells must also demonstrate that they can bind weakly to some human protein fragments. Only a tiny percentage of T cells pass these tests and are allowed to leave the thymus and circulate in the body to defend against viruses, other diseases, and cancerous cells.
Inside the thymus, T cells are exposed to “self-peptides” — small human protein fragments — bound to HLA proteins. Chakraborty and co-workers had previously shown that the diversity of self-peptide fragments presented in the thymus influences the kinds of T cells a person can produce. The type and number of self-peptides expressed are determined by the HLA genes, which have hundreds of distinct forms, including HLA B57. Each person carries up to six of them (three inherited from each parent).
Using data from previous studies, the Ragon team found that HLA B57 protein presents fewer types of self-peptides than most other HLA proteins. (HLA B27 is another protein that presents few types of self-peptides and also appears to protect against HIV and promote autoimmune disorders.) In this study, Chakraborty and postdoctoral fellow Elizabeth Read and graduate student Andrej Kosmrlj, lead authors of the paper, used their computer model to study what happens when maturing T cells are exposed to only a small diversity of self-peptides in the thymus.
T cells with receptors that bind strongly to any of the self-peptides in the thymus are forced to undergo cell suicide, because of their potential to attack the body’s own cells. Chakraborty and co-workers showed that this means that, for most individuals, most of the body’s T cells have receptors that bind to targeted viral proteins via a number of weak interactions, with each interaction making a significant contribution to the binding. Thus, a single mutation to an HIV peptide can potentially evade the immune response.
A different scenario unfolds in people who have the HLA B57 gene. Using their computer model, Chakraborty and colleagues showed that, because those individuals’ T cells are exposed to fewer self-peptides in the thymus, T cells with receptors that mediate strong binding to viral proteins via just a few important contacts are more likely to escape the thymus. This makes these T cells more cross-reactive to targeted HIV peptide mutants, because as long as those points in the viral proteins don’t mutate, the T cells are still effective. The model also showed that once those T cells are released into the bloodstream, they can effectively attack HIV proteins, even when the virus mutates.
This model also explains why people with the HLA B57 gene have autoimmune problems: Their T cells are more likely to bind strongly to human peptides not encountered in the thymus.
The computational studies explained many puzzles, but also made a prediction: Individuals with HLA genes that result in a display of fewer self-peptides should control HIV (and other viruses like hepatitis C virus) better. To test this prediction, the researchers studied nearly 2,000 patients — 1,100 “HIV controllers” and 800 who progressed normally to AIDS, and confirmed that this appears to be true.
‘A horrific global problem’
The melding of complementary approaches — clinical studies, basic immunology and computations rooted in engineering and the physical sciences — exemplified by this study is part of the mission of the Ragon Institute, founded last year to support discovery of an effective AIDS vaccine.
The idea is to break down the “scientific silos” in which many researchers work, says Walker. “Because of the Ragon funding, Arup and I had a conversation we never would have otherwise had,” he says. “We probably never would have met.”
There are now a few dozen researchers working on Ragon-funded HIV studies, and Walker believes those new collaborations can lead to many more successes. “There are people out there who have never worked on HIV problems that have something to immediately contribute, and this is a great example of that,” he says. “We have not yet brought the full potential of scientific knowledge to bear on trying to do something about HIV, which remains a horrific global problem.”
The research was also partly funded by Chakraborty’s NIH Director’s Pioneer Award. “Combining fundamental understanding of molecular mechanisms underlying immune function with computational methods for scanning large numbers of sequences allowed the development of a powerful explanation for a problem of great importance to public health. Such interdisciplinary research results are one of the goals of the NIH Director’s Pioneer Award program,” says Jeremy M. Berg, director of the National Institute of General Medical Sciences.