Statistics for neurological disorders are grim. More than a million Americans suffer from Parkinson's disease alone -- a number that is expected to soar over the next few decades as the population ages. No current therapies alter the fundamental clinical course of the condition.
Now, scientists at MIT and the Whitehead Institute, in collaboration with colleagues at several research centers including the University of Missouri, have identified a key biological pathway that, when obstructed, causes Parkinson's symptoms. Even more importantly, they have figured out how to repair that pathway and restore normal neurological function in certain animal models.
"For the first time we've been able to repair dopaminergic neurons, the specific cells that are damaged in Parkinson's disease," said MIT biology professor, Whitehead member and Howard Hughes Medical Institute investigator Susan Lindquist, senior author on a paper published June 22 online in Science.
In 2003, researchers in the Lindquist lab described using yeast cells as "living test tubes" in which they could study Parkinson's. They reported that when a Parkinson's-related protein called alpha-synuclein was overexpressed in these cells, clumps of misshapen proteins gathered, and in many cases the cells either became sick or died.
Aaron Gitler and Anil Cashikar, postdoctoral researchers in the Lindquist lab, decided to follow up on these results by asking a simple question: Is it possible to rescue these cells when an overexpression of alpha-synuclein would normally make them sick?
They began with an array of yeast cells in which each cell overexpressed one particular gene. This array, prepared by scientists at the Harvard Institute of Proteomics, covers the entire yeast genome. All cells were also infected with alpha-synuclein. They reasoned that if they identified genes whose overexpression rescued a cell, that would tell them something about how alpha-synuclein made the cell sick in the first place.
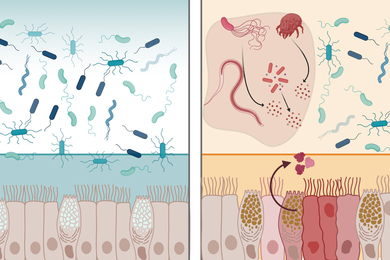
Most of the proteins that they identified pointed to a pathway that involves two cellular organelles, the endoplasmic reticulum (ER) and the Golgi. The ER is the cell's protein factory, where proteins assume their requisite shapes. Once a protein has properly folded, it is trafficked over to the Golgi, where it is fine-tuned and further prepared for its designated task.
Working with Antony Cooper from the University of Missouri, Kansas City, Lindquist's team demonstrated that when alpha-synuclein becomes mutated and clumps at the cell surface, it manages to drag away a protein that helps transport between the ER and the Golgi. Proteins are blocked from navigating this crucial route, and the cell dies.
This isn't just a general toxic effect caused by any misfolded protein. It is specific to alpha-synuclein, the protein associated with Parkinson's disease.
"All this was done in yeast," said Gitler. "Our next goal was to find out what this told us about actual neurons."
If mutations of alpha-synuclein dragged the ER/Golgi transport protein away from doing its job, as the yeast research indicated, then cell death might be averted simply by increasing the levels of this transport protein. Working with colleagues at University of Pennsylvania, University of Alabama and Purdue University, the consortium tested this hypothesis in the fruit fly, C. elegans worm, and in neurons culled from rats -- all of which had alpha-synuclein-induced Parkinson's symptoms. In every case, symptoms were reversed by increasing levels of this transport protein.
"We tried this a number of different ways, from creating transgenic animals that naturally overexpressed this protein, to injecting a copy of the gene for this transport protein into the neurons through a gene-therapy technique," said Gitler. "In all cases the results were the same. Cell death ceased, and the neurons were restored to normal health."
"Protein folding problems are universal, so we hoped we could use these simple model organisms to study something as deeply complex as neurodegenerative disease," Lindquist said. "Most people thought we were crazy. But we now not only have made progress in understanding this dreadful disease, but we have a new platform for screening pharmaceuticals."
"This gives a whole new direction for understanding what's been going wrong in these patients and for considering much better strategies for treating people," Cooper said.
This work was supported by the National Institutes of Health.