Our brains constantly work to make predictions about what’s going on around us to ensure that we can attend to and consider the unexpected, for instance. A new study examines how this works during consciousness and also breaks down under general anesthesia. The results add evidence to the idea that conscious thought requires synchronized communication — mediated by brain rhythms in specific frequency bands — between basic sensory and higher-order cognitive regions of the brain.
Previously, members of the research team in The Picower Institute for Learning and Memory at MIT and at Vanderbilt University had described how brain rhythms enable the brain to remain prepared to attend to surprises. Cognition-oriented brain regions (generally at the front of the brain) use relatively low-frequency alpha and beta rhythms to suppress processing by sensory regions (generally toward the back of the brain) of stimuli that have become familiar and mundane in the environment (e.g., your co-worker’s music). When sensory regions detect a surprise (e.g., the office fire alarm), they use faster-frequency gamma rhythms to tell the higher regions about it, and the higher regions process that at gamma frequencies to decide what to do (e.g., exit the building).
The new results, published Oct. 7 in the Proceedings of the National Academy of Sciences, show that when animals were under propofol-induced general anesthesia, a sensory region retained the capacity to detect simple surprises but communication with a higher cognitive region toward the front of the brain was lost, making that region unable to engage in its “top-down” regulation of the activity of the sensory region and keeping it oblivious to simple and more complex surprises alike.
What we've got here is failure to communicate
“What we are doing here speaks to the nature of consciousness,” says co-senior author Earl K. Miller, Picower Professor in The Picower Institute for Learning and Memory and MIT’s Department of Brain and Cognitive Sciences. “Propofol general anesthesia deactivates the top-down processes that underlie cognition. It essentially disconnects communication between the front and back halves of the brain.”
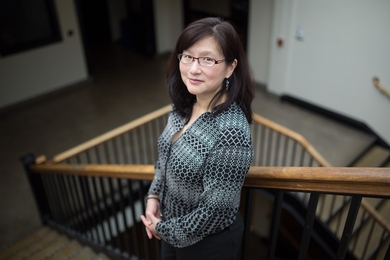
Co-senior author Andre Bastos, an assistant professor in the psychology department at Vanderbilt and a former member of Miller’s MIT lab, adds that the study results highlight the key role of frontal areas in consciousness.
“These results are particularly important given the newfound scientific interest in the mechanisms of consciousness, and how consciousness relates to the ability of the brain to form predictions,” Bastos says.
The brain’s ability to predict is dramatically altered during anesthesia. It was interesting that the front of the brain, areas associated with cognition, were more strongly diminished in their predictive abilities than sensory areas. This suggests that prefrontal areas help to spark an “ignition” event that allows sensory information to become conscious. Sensory cortex activation by itself does not lead to conscious perception. These observations help us narrow down possible models for the mechanisms of consciousness.
Yihan Sophy Xiong, a graduate student in Bastos’ lab who led the study, says the anesthetic reduces the times in which inter-regional communication within the cortex can occur.
“In the awake brain, brain waves give short windows of opportunity for neurons to fire optimally — the ‘refresh rate’ of the brain, so to speak,” Xiong says. “This refresh rate helps organize different brain areas to communicate effectively. Anesthesia both slows down the refresh rate, which narrows these time windows for brain areas to talk to each other and makes the refresh rate less effective, so that neurons become more disorganized about when they can fire. When the refresh rate no longer works as intended, our ability to make predictions is weakened.”
Learning from oddballs
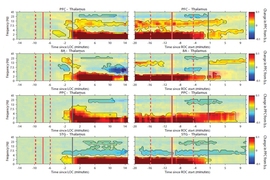
To conduct the research, the neuroscientists measured the electrical signals, “or spiking,” of hundreds of individual neurons and the coordinated rhythms of their aggregated activity (at alpha/beta and gamma frequencies), in two areas on the surface, or cortex, of the brain of two animals as they listened to sequences of tones. Sometimes the sequences would all be the same note (e.g., AAAAA). Sometimes there’d be a simple surprise that the researchers called a “local oddball” (e.g., AAAAB). But sometimes the surprise would be more complicated, or a “global oddball.” For example, after seeing a series of AAAABs, there’d all of a sudden be AAAAA, which violates the global but not the local pattern.
Prior work has suggested that a sensory region (in this case the temporoparietal area, or Tpt) can spot local oddballs on its own, Miller says. Detecting the more complicated global oddball requires the participation of a higher order region (in this case the frontal eye fields, or FEF).
The animals heard the tone sequences both while awake and while under propofol anesthesia. There were no surprises about the waking state. The researchers reaffirmed that top-down alpha/beta rhythms from FEF carried predictions to the Tpt and that Tpt would increase gamma rhythms when an oddball came up, causing FEF (and the prefrontal cortex) to respond with upticks of gamma activity as well.
But by several measures and analyses, the scientists could see these dynamics break down after the animals lost consciousness.
Under propofol, for instance, spiking activity declined overall but when a local oddball came along, Tpt spiking still increased notably but now spiking in FEF didn’t follow suit as it does during wakefulness.
Meanwhile, when a global oddball was presented during wakefulness, the researchers could use software to “decode” representation of that among neurons in FEF and the prefrontal cortex (another cognition-oriented region). They could also decode local oddballs in the Tpt. But under anesthesia the decoder could no longer reliably detect representation of local or global oddballs in FEF or the prefrontal cortex.
Moreover, when they compared rhythms in the regions amid wakeful versus unconscious states they found stark differences. When the animals were awake, oddballs increased gamma activity in both Tpt and FEF and alpha/beta rhythms decreased. Regular, non-oddball stimulation increased alpha/beta rhythms. But when the animals lost consciousness the increase in gamma rhythms from a local oddball was even greater in Tpt than when the animal was awake.
“Under propofol-mediated loss of consciousness, the inhibitory function of alpha/beta became diminished and/or eliminated, leading to disinhibition of oddballs in sensory cortex,” the authors wrote.
Other analyses of inter-region connectivity and synchrony revealed that the regions lost the ability to communicate during anesthesia.
In all, the study’s evidence suggests that conscious thought requires coordination across the cortex, from front to back, the researchers wrote.
“Our results therefore suggest an important role for prefrontal cortex activation, in addition to sensory cortex activation, for conscious perception,” the researchers wrote.
In addition to Xiong, Miller, and Bastos, the paper’s other authors are Jacob Donoghue, Mikael Lundqvist, Meredith Mahnke, Alex Major, and Emery N. Brown.
The National Institutes of Health, The JPB Foundation, and The Picower Institute for Learning and Memory funded the study.