An artificial intelligence program that’s better than human doctors at recommending treatment for sepsis may soon enter clinical trials in London. The machine learning model is part of a new way of practicing medicine that mines electronic medical-record data for more effective ways of diagnosing and treating difficult medical problems, including sepsis, a blood infection that kills an estimated 6 million people worldwide each year.
The discovery of a promising treatment strategy for sepsis didn’t come about the regular way, through lengthy, carefully-controlled experiments. Instead, it emerged during a free-wheeling hackathon in London in 2015.
In a competition bringing together engineers and health care professionals, one team hit on a better way to treat sepsis patients in the intensive-care unit, using MIT’s open-access MIMIC database. One team member, Matthieu Komorowski, would go on to work with the MIT researchers who oversee MIMIC to develop a reinforcement learning model that predicted higher survival rates for patients given lower doses of IV fluids and higher doses of blood vessel-constricting drugs. The researchers published their findings this fall in Nature Medicine.
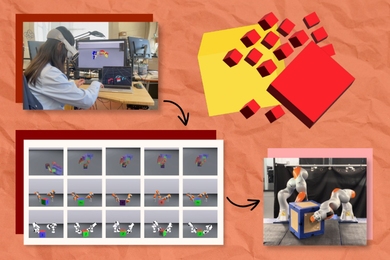
The paper is part of a stream of research to come out of the “datathons” pioneered by Leo Celi, a researcher at MIT and staff physician at Beth Israel Deaconess Medical Center. Celi held the first datathon in January 2014 to spark collaboration among Boston-area nurses, doctors, pharmacists and data scientists. Five years later a datathon now happens once a month somewhere in the world.
Following months of preparation, participants gather at a sponsoring hospital or university for the weekend tocomb through MIMIC or a local database in search of better ways to diagnose and treat critical care patients. Many go on to publish their work, and in a new milestone for the program, the authors of the reinforcement learning paper are now preparing their sepsis-treatment model for clinical trials at two hospitals affiliated with Imperial College London.
As a young doctor, Celi was troubled by the wide variation he saw in patient care. The optimal treatment for the average patient often seemed ill-suited for the patients he encountered. By the 2000s, Celi could see how powerful new tools for analyzing electronic medical-record data could personalize care for patients. He left his job as a doctor to study for a dual master’s in public health and biomedical informatics at Harvard University and MIT respectively.
Joining MIT’s Institute for Medical Engineering and Science after graduation, he identified two main barriers to a data revolution in health care: medical professionals and engineers rarely interacted, and most hospitals, worried about liability, wanted to keep their patient data — everything from lab tests to doctors’ notes — out of reach.
Celi thought a hackathon-style challenge could break down those barriers. The doctors would brainstorm questions and answer them with the help of the data scientists and the MIMIC database. In the process, their work would demonstrate to hospital administrators the value of their untapped archives. Eventually, Celi hoped that hospitals in developing countries would be inspired to create their own databases, too. Researchers unable to afford clinical trials could understand their own patient populations and treat them better, democratizing the creation and validation of new knowledge.
“Research doesn’t have to be expensive clinical trials,” he says. “A database of patient health records contains the results of millions of mini experiments involving your patients. Suddenly you have several lab notebooks you can analyze and learn from.”
So far, a number of sponsoring hospitals — in London, Madrid, Tarragona, Paris, Sao Paulo, and Beijing — have embarked on plans to build their own version of MIMIC, which took MIT’s Roger Mark and Beth Israel seven years to develop. Today the process is much quicker thanks to tools the MIMIC team has developed and shared with others to standardize and de-identify their patient data.
Celi and his team stay in touch with their foreign collaborators long after the datathons by hosting researchers at MIT, and reconnecting with them at datathons around the globe. “We’re creating regional networks — in Europe, Asia and South America — so they can help each other,” says Celi. “It’s a way of scaling and sustaining the project.”
Humanitas Research Hospital, Italy’s largest, is hosting the next one — the Milan Critical Care Datathon Feb. 1-3 — and Giovanni Angelotti and Pierandrea Morandini, recent exchange students to MIT, are helping to put it on. “Most of the time clinicians and engineers speak different languages, but these events promote interaction and build trust,” Morandini says. “It’s not like at a conference where someone is talking and you take notes. You have to build a project and carry to it to the end. There are no experiences like this in the field.”
The pace of the events has picked up with tools like Jupyter Notebook, Google Colab, and GitHub letting teams dive into the data instantly and collaborate for months after, shortening the time to publication. Celi and his team now teach a semester-long course at MIT, HST.953 (Collaborative Data Science in Medicine), modeled after the datathons, creating a second pipeline for this kind of research.
Beyond standardizing patient care and making AI in health care accessible to all, Celi and his colleagues see another benefit of the datathons: their built-in peer-review process could prevent more flawed research from being published. They outlined their case in a 2016 piece in Science Translational Medicine.
“We tend to celebrate the story that gets told — not the code or the data,” says study co-author Tom Pollard, an MIT researcher who is part of the MIMIC team. “But it’s the code and data that are essential for evaluating whether the story is true, and the research legitimate.”