During the first 24 hours of invasion by the malaria-inducing parasite Plasmodium falciparum, red blood cells start to lose their ability to deform and squeeze through tiny blood vessels--one of the hallmarks of the deadly disease that infects nearly 400 million people each year. Now, an international team of researchers led by an MIT professor has demonstrated just why that happens.
By knocking out the gene for a parasite protein called RESA (ring-infected erythrocyte surface antigen), the researchers found that the protein, transferred from the parasite to the cell's interior molecular network, causes red blood cells to become less deformable.
"This is the first time a particular protein has been shown to have such a large effect on red blood cell deformability," said Subra Suresh, Ford Professor of Engineering and senior author of a paper on the work appearing in the online edition of the Proceedings of the National Academy of Sciences the week of May 21.
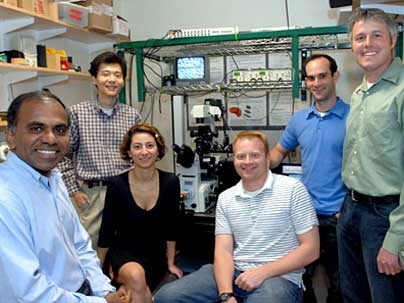
The work, a collaboration between researchers at MIT, the Institut Pasteur in Paris, France and the National University of Singapore, could ultimately lead to the development of treatments that target the parasite protein.
Suresh, who holds appointments in materials science and engineering, biological engineering, mechanical engineering and the Harvard-MIT Division of Health Sciences and Technology, has been studying the mechanics of red blood cells and the effects of malaria on those cells for several years.
When the malaria parasite, Plasmodium falciparum, infects red blood cells, the blood cells lose their ability to deform and eventually clump together and get stuck in tiny blood vessels, or capillaries.
The RESA protein has long been suspected to be involved in the early stages of that process. The parasite produces RESA during the first stage of malaria (known as the ring stage) and then transports it to the cell surface.
In this experiment, the researchers cloned the parasite and then knocked out the gene that produces RESA and then measured the red blood cells' deformability with "optical tweezers," which use lasers to stretch cell membranes.
They found that in red blood cells infected by parasites without RESA, deformability remained normal during the first 24 hours of infection. In other parasites where RESA was turned back on after being knocked out, deformability was affected just as it was by (wild type) parasites in which RESA was never knocked out.
"That the deformability changed several-fold was a big surprise," said Suresh.
Because malaria patients usually experience high fever episodes, the researchers also performed their experiments at fever temperatures (about 41 degrees Celsius), as well as normal body temperature (37 degrees Celsius). They found that RESA has a much greater impact on deformability at fever temperatures.
The research team believes that when RESA travels to the cell membrane, it binds to the cell's cytoskeleton--a scaffolding of proteins that lies just inside the cell membrane. In a paper published earlier this year, Suresh and colleagues demonstrated that healthy red blood cells' ability to deform depends on the structure of this network. (See web.mit.edu/newsoffice/2007/blood.html)
When the bonds in the protein network are broken, holes open up in the cytoskeleton, allowing the cell to become more fluidic and squeeze through narrow passages. But when RESA binds to the network, it likely interferes with the proteins' ability to break and form bonds with each other, decreasing deformability, according to Suresh. In an unrelated parallel study, researchers at the New York Blood Center and their collaborators have recently identified specific sites in the red cell cytoskeleton to which RESA binds.
In future studies, the researchers plan to study the effects of proteins produced by the malaria parasite during later stages of infection. They also plan to look at whether the RESA protein plays any role in why another strain of the malaria parasite, Plasmodium vivax, is less lethal than P. falciparum.
The collaboration between MIT and the Institut Pasteur began with a serendipitous encounter: In a crowded cafeteria at the École des Mines in Paris, where Suresh was visiting a few years ago, he met a colleague from Institut Pasteur. She introduced him to the researchers studying malaria at Pasteur, who included microbiologist Monica Diez-Silva, now an MIT and GEM4 postdoctoral fellow and a lead author of the PNAS paper.
Shortly after this meeting, Suresh started a formal collaboration known as GEM4 (Global Enterprise for MicroMechanics and Molecular Medicine), which brings together researchers from MIT, Institut Pasteur, the National University of Singapore and other universities around the world. This year, GEM4 will holds its second summer school, where scientists learn about one another's work and form research partnerships. This GEM4 activity is supported by a number of institutions, including the National Science Foundation.
Multidisciplinary, multinational research at the intersections of engineering, life sciences and medicine, with major implications for public health is "exactly what GEM4 was designed to facilitate and accomplish," Suresh said.
Lead authors of the PNAS paper are Diez-Silva and John P. Mills, both postdoctoral associates in materials science and engineering. Other MIT authors are David J. Quinn, graduate student in mechanical engineering; Ming Dao, research scientist in materials science and engineering; and Matthew Lang, assistant professor of biological engineering and mechanical engineering. Authors from Institut Pasteur are Genevieve Milon, Peter H. David, Odile Mercereau-Puijalon and Serge Bonnefoy. Authors from the National University of Singapore are Kevin S.W. Tan and Chwee Teck Lim.
The research was funded by an interuniversity grant received by GEM4, a Pasteur Institut research grant, Agence Nationale de Recherche sur le Sida, the National University of Singapore and the Computational Systems Biology Program of the Singapore-MIT Alliance.
A version of this article appeared in MIT Tech Talk on May 23, 2007 (download PDF).