Introduction
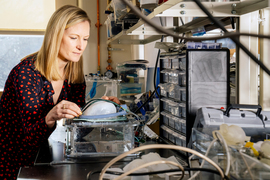
Ellen Roche is an associate professor of mechanical engineering and the associate head of the Department of Mechanical Engineering at MIT. Her research team develops new devices and therapeutic strategies for repairing the heart and other tissues. Here, she speaks with MIT President Sally Kornbluth about her work, the advantages of taking a nonlinear route to one’s chosen career, and the importance of saying “yes” to unexpected opportunities.
Links
Timestamps
Transcript
Sally Kornbluth: Hello, I'm Sally Kornbluth, president of MIT, and I'm thrilled to welcome you to this MIT community podcast, Curiosity Unbounded. Since I arrived at MIT, I've been particularly inspired by talking with members of our faculty who recently earned tenure. Like their colleagues in every field here, they're pushing the boundaries of knowledge. Their passion and their brilliance, their boundless curiosity, offer a wonderful glimpse of the future of MIT.
Today, my guest is Ellen Roche. Ellen is an associate professor in the Department of Mechanical Engineering. Her work focuses on mechanical devices and biomaterials with medical applications. She also directs the Therapeutic Technology Design and Development Lab at MIT. Now, because so much of what happens here at MIT happens in the labs, I wanted to bring Ellen on to the podcast to talk about how lab work translates to the real world. Ellen, thank you for being here today.
Ellen Roche: Thank you for having me. It's a pleasure.
Sally Kornbluth: You have worked on a biorobotic heart. This heart, I was looking forward to hearing more about this, talking to you about it. As I understand it, in 2020, your lab developed a heart that's described as being like the real thing. Then COVID happened, and your lab, like many at MIT, had to close. Then when your lab reopened, the work continued. I believe you actually improved on the heart by turning to 3D printing. Tell me a little bit about the story of this heart. How did it get started? Where are you now? Where are you hoping to go with it?
Ellen Roche: I guess the work started during my doctoral work at Harvard. I did my PhD there. I worked on a device that was an implantable device that went around a heart like a sock or a sleeve that would be implanted around a failing heart in a person with heart failure. It would act to give an extra assistance to the heart muscle to pump enough blood around the body. That was really the first configuration or version of the soft robotic heart devices.
When I started my group here at MIT, I continued that work a little bit and we made a textile sleeve. We showed that that could work even better than the original version. Then I thought, "How can we use this technology to develop better test beds on the bench?" So that we can recreate the motion and the biomechanics of the heart on the bench to allow for better testing of devices like heart valves and implantable devices that go inside the heart, and you want to test them in a very realistic setting.
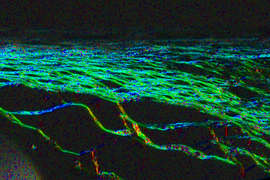
The first version in 2020, it was led by my first graduate student, or actually second, but first mechanical engineering graduate student, Clara. We took an explanted pig heart. Pig hearts are similar sizes to human hearts. We removed all the dead or stiffened muscle from the heart but preserved all the intracardiac features, so all the heart valves and everything inside the heart was kept intact. We used a very specific dissection process, unraveled the muscle from around the heart, and then we replaced that with a synthetic soft robotic muscle that we could tune and control and then we could basically make the heart beat again on the bench. Then you can put cameras in and sensors on it and you can measure flows and pressures. You can recreate the heart motion, the pumping function, the valve motion, so really bringing the heart back to life on the bench. That was where it started and we used it to test a number of devices.
Some of the issues with that are that it's real tissue, so there's a certain shelf life. We did some work on coming up with methods to keep it functioning for longer, but you still have some limitations. Then we thought, "Maybe we can fully 3D print a heart." We take a patient's scan and get the exact anatomy and then we use advanced 3D printers. The technology has advanced so much in recent years. We print in a soft material so we can match exactly the anatomy of a given patient. Diseased patients, some have congenital heart defects that are very different anatomies. Then we can use our soft robotic technologies to make a sleeve that goes around it or to create a band that goes around the vessel so we can create narrowing. Then we have this pumping heart on the bench again, but we can create different disease types and we can tune them. We can use them to learn more about the biomechanics to test devices. With that, then we can print different edge cases of anatomies. We can look at various different devices and tune it depending on what we're trying to test.
Now moving forward, we think, "How about moving towards printing an entire total artificial heart?" We're way away from that now, but if we can do that, you can envision the people who are at end-stage heart failure that are waiting for a transplant and on these long lists could actually have a printed, entirely synthetic, beating heart that has active motion and everything that replicates their own native heart.
Sally Kornbluth: That's pretty incredible. It seems then that in the current state, for example, if a patient needs a particular assistive device, you can see how it will interact with their own physiology. In your original work, the sleeve work that you did as a graduate student, was that ever actually deployed clinically?
Ellen Roche: Not yet, no. I think for this type of—class III is the highest risk medical device—the regulatory approval takes a lot of time, as it should. I think that would take quite a bit of work to advance that to be implanted in humans. Part of the reason for the pivot towards these benchtop models was because you can deploy them quicker and they can be used and translated in industry a lot quicker than a very high-risk device. But we're still trying to pursue both in parallel. Some have nearer-term goals than the long-term implant.
Sally Kornbluth: I guess, also, correct me if I'm wrong, but the artificial hearts could be used for models in particular, patients can be used by surgeons to map out their approach, for instance, if someone has an unusual anatomy.
Ellen Roche: Absolutely. Recently, we were approached by one of the local hospitals to build some models in the hospitals to train their surgeons or their attendings to study which type of pump to use, which type of left ventricular assist device, and to tune the parameters and vary them and see that in real time. The surgeon that came actually to visit the lab had seen some of the work. His mom actually had seen it and called him, and was like, "You need to meet these people." He came and was excited and we're trying to set that up.
Sally Kornbluth: Oh, fun. If you succeed in making an entirely artificial heart that could actually be implanted, what sort of materials do you envision being used there?
Ellen Roche: That's one of the big challenges, of course. They have to be biocompatible, but they have to be very robust because the heart beats…
Sally Kornbluth: A lot.
Ellen Roche: … 72 times a minute on average. A lot of the research is going into that. Of course, the material that contacts the blood as well has to be designed very specifically, because you don't want to cause clotting. We didn't have that issue with the sleeve because it was non-blood contacting, but if it's a total artificial heart, we will.
Sally Kornbluth: Then you get fibrosis sometimes around, that destroys the blood flow, et cetera.
Ellen Roche: Exactly, yes. Depending on what part of the device, we may have to functionalize in different ways. But there's a lot of existing implants that are proven blood-contacting. The goal at the moment is if we can build the active structure but use approved prosthetic valves that are already implanted and have been implanted in human hearts before and haven't had issues. If we can use materials to align the internal surface of the heart that have been used in vascular grafts or blood-contacting devices, we can at least de-risk parts of it and then we would be controlling the pumping function.
Sally Kornbluth: That's really interesting. I've heard also that another recent project in your lab concerns hydrogels that can repair or replace diseased tissues. Can you tell us about that work? Maybe starting from exactly what are hydrogels for the audience, and going through how they might be deployed.
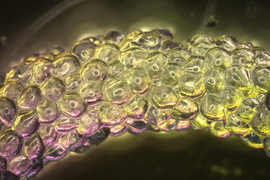
Ellen Roche: There's a lot of advancements in the overall hydrogel field recently. This particular gel that we're working on, it's a biopolymer. It has these unique mechanical properties where it's shear thinning, so we can deliver it through a long tube. But then when it comes out of the tube or the catheter, it solidifies, so it's like this phase changing. It's called a granular hydrogel. Small little spheres, basically. This is in collaboration with Jennifer Lewis at Harvard who does a lot of work in bioprinting and soft materials. My lab is interested in implantable devices for the heart, so we thought, "Can we use this material and use a catheter to deliver it?" A catheter is a long tube that's inserted into the body so you can do minimally invasive procedures. We thought, "Can we use this material to occlude part of the heart where clots can form and cause a stroke in patients that have arrhythmia or atrial fibrillation?" There's this little tiny part of the heart called the left atrial appendage. It's like a little outpouching from the upper chamber of the heart. If a patient has atrial fibrillation in the upper chambers of their heart, you're kind of quivering. You get blood stasis in that area and clots can form. 90% of stroke-causing clots form there. If we can occlude it, it prevents clots from forming there, from going to the brain and causing a stroke.
Sally Kornbluth: You actually are rerouting things. You stop the blood from actually going into that…
Ellen Roche: This one cul-de-sac or dead end.
Sally Kornbluth: Got it.
Ellen Roche: You can put the tube up through the leg. It's minimally invasive. You cross the septum of the heart and then you can fill that part. It basically blocks it off from the blood flow. The advantage of using a hydrogel biological material like that, first you can deliver it, it will stabilize, and then the patient's tissue will grow over it. Then the only thing in contact with the blood is the patient's own tissue after a certain amount of time.
Sally Kornbluth: How about babies who were born, for instance, with a congenital hole between chambers? Could you envision using it for something like that?
Ellen Roche: Absolutely, yes. That's one of the uses we have envisioned for it. We have other work in the lab, again, some from my doctoral work and some in the lab, where we design these biopolymeric patches that can be adhered to the septum of the heart to close these holes either in babies or in adults. Sometimes there is a defect that isn't problematic unless you're prone to clotting, because then you can get clots.
Sally Kornbluth: Right. You can also throw clots there.
Ellen Roche: Right, exactly. We're working on these kinds of patches and adhesives that can work in the blood. We had a light-activated adhesive delivered by a catheter that could cure this patch onto the septum of the heart.
Sally Kornbluth: You would laser cure it or something?
Ellen Roche: Yes. We used blue light. You could activate this adhesive to adhere to the septum, so a Coda patch adhesive and then two balloons, and one was reflective to reflect the light. There was a fiber optic in the catheter. The light would reflect back and cure the patch onto the septum. It was flexible and elastomeric and blood compatible and then you'd take out the catheter, so it would just be this patch. Again, the goal is the patient's tissue grows over it. That one we licensed to a startup company in France, in Paris. They were working on it for a while and they're still pursuing this defect closure as well.
Sally Kornbluth: Very interesting. As I understand it, earlier in your career, you worked in the medical device industry. What motivated you to make the jump from industry to academia?
Ellen Roche: I think when I started in industry, I was really eager to get some experience after undergrad. There was a program in Ireland at the time, which was a graduate program, to do some time in an Irish company and then some time in a sister company abroad, so that brought me to the U.S. When I started that, I thought I'll do some industry experience, but I always knew I wanted to do further study, a master's or a PhD.
That program brought me to California and I ended up getting involved in a project there in Abbott Vascular, where we were working on a system for getting regulatory approval for one of their stents. Then I ended up there four years instead of six months. Really enjoyed it, I loved the work, but then I still had that desire to do further study and learn new technologies that could be applied to devices. I was working in cardiac devices in industry and loved that part of it, but I thought maybe there's more I can learn and different techniques and approaches that I could use and have this open space to be creative and try different things. There was a certain point where I was employed still on an expatriate contract from Ireland and they closed one of the sites in Galway. At that point, they were like, "You can either switch to a U.S. contractor or take a redundancy package," and I was like, "That's perfect. This is a good chance." I traveled for a while and then I started a master's first. It was a master's I could do while working, so I worked in Medtronic, and then I said, "Okay, I'm into the research again." I applied for a PhD through a Fulbright science and technology program and then came to Harvard.
Sally Kornbluth: Fantastic. I'm just curious, your own PhD students now, what's the split of students who are going to industry versus have aspirations for an academic career?
Ellen Roche: That's a great question. I'm six years here, so I just…
Sally Kornbluth: They're just starting.
Ellen Roche: They're starting. My eighth graduate student defended yesterday, so that was exciting. To date, I would say there is probably more of the students have gone to industry, but a couple have stayed in academia. Then a lot of the postdocs that have been in my lab have stayed in academia. Overall, I would say probably 50/50. But I really do encourage them all to have some sort of industry experience during their PhD. I feel like we're developing these devices that are implanted in humans and it's really important to understand all that happens between designing them in the lab and proving that they work to actually getting them into a person. There's so much regulatory things. The design of the trial, the manufacturing. There's so much that's very hard to even imagine until you spend some time in industry. So most of my students have done an internship.
Sally Kornbluth: That's great.
Ellen Roche: Yes. One of my students, Keegan, she's actually went to med school after she defended her PhD, but she spent time in Boston Scientific setting up some of the models she developed. Other students spent time working with Dassault Systèmes who do computer aided design and computational modeling. We have quite a few industry-sponsored projects now in the lab, so I think it's a good opportunity for the students to be in an academic setting, but work very closely with industry personnel as well. That can help them to figure out, "Do I want to go the industry route or the academic route?"
Sally Kornbluth: Also having realistic expectations. As you're saying, knowing that the steps from conceiving an idea and showing that it works on a lab bench, to actually getting it into a human, is a lot of hurdles and a very long path. Speaking of students, I think I often hear from faculty that what drew them to MIT is the quality of the students. Talk a little bit more about your experience collaborating with the students here, how you've found it.
Ellen Roche: It's amazing. I'm so lucky to get to work with such talented students. They really just impress me every day with how creative they are, and diligent and collaborative. Because my work is interdisciplinary, I have students from mechanical engineering and then I have a lot of students from the HST program [Harvard-MIT Health Sciences and Technology] because I'm core faculty in IMES [Institute for Medical Engineering and Science] as well. They have very different backgrounds, but I love seeing how they work together to solve these problems. It's just a privilege to work with them as well in teaching. You teach these classes and the students, they're so eager to learn. They just ask such smart, intelligent questions, and they want more hours in the lab. It's just fantastic.
Sally Kornbluth: For our listeners, our HST program in collaboration with Harvard produces future clinician scientists, students who are doing MD-PhDs. This area of research seems like a perfect training ground and future career arena for students who are really interested in doing fundamental research but making a clinical difference.
Ellen Roche: Absolutely, yes.
Sally Kornbluth: Some of your work is actually computational as well, so computational modeling. I'm wondering, first of all, how AI affects what you're doing and how it's affecting the field, but I'm also curious how you personally learned what you needed to learn to be able to apply these computational approaches?
Ellen Roche: I did my postdoc in computational modeling. We look at modeling the motion of the heart, the fluid-structure interaction, basically how the blood flows in response to the contraction of the heart, and how, when you implant devices, that can change the mechanics of the heart and how the devices are affected by this three-dimensional motion. I learned a lot of finite element models and different computational models to study that. We have a subgroup in the lab that work almost exclusively on computational models. More recently, I would say, we've looked at using some AI methods to take multiple patient data sets, images, and try to make these synthetic anatomical models where we can parameterize different parts of the heart and look at different anatomies and create these data-driven surrogates so we can do finite element models much quicker. I think that will help us to use these to inform clinical practice. You could imagine you go for a scan, an MRI scan, and then you have this digital twin that is your own beating heart, and then you can say like, "If there's an issue, this will be how your heart will perform if you have this intervention." Or if you are trying to inform a patient about what will happen if they don't make certain lifestyle changes.
Sally Kornbluth: You can show them what will happen if their arteries become occluded.
Ellen Roche: Right. "Here's your heart now…"
Sally Kornbluth: "Here's your heart on donuts."
Ellen Roche: Exactly. Because you could have age matched and lifestyle matched virtual twins, and with our work in the lab, we could also do physical twins. "Here's your heart beating right now, and if we put in this LVAD, you'll get this much more output. Or if you don't do anything, it's going to remodel and it's going to grow." A lot of the computational work we were doing, as well, is looking at how the heart muscle adapts to various pressure overloads or volume overloads. Over time, the heart will remodel, which is fascinating. It'll grow and change shape and these computational models can predict that.
Sally Kornbluth: That's really interesting. I would think, also, people are obviously sometimes hesitant to undergo heart surgery and wondering what the ultimate benefit will be. But if you can say, as you said, "If you put in this device or you make this surgical modification or what have you, this is what we predict in terms of the heart output."
Ellen Roche: Yes, absolutely. As well as patient education and, "Here's why we're doing what we're doing," it can also help the surgeons to decide, "If we use this continuous flow pump versus this pulsatile pump, here's what it will look like or here's a way we can fit it."
Sally Kornbluth: I'm just curious, and you may not have a good answer to this, I'm just curious whether there are colleagues in related fields that are, in a sense, doing the same things with other organs. In other words, 3D printing. It seems a little bit different because so much of the heart function is based on large architecture as opposed to filtration capacity, let's say, in a kidney or in a liver.
Ellen Roche: Yes. There definitely is. Even within my group, we've thought about, "How can we translate this technology to other organs or tissues?" We have actually developed an assist device for the diaphragm. Like the heart, it's a large contracting muscle. It's life sustaining, it's mechanical, so we have developed these actuators or artificial muscles that go above the diaphragm and help to augment the downward motion of the diaphragm to help with inspiration in patients that have muscular dystrophy or disorders.
Sally Kornbluth: Or ALS or other neurodegenerative disorders. That's really interesting.
Ellen Roche: Yes. That was another obvious type of large mechanically-driven composite structure where we could augment the native function without overtaking it. There are other groups developing, as well, anatomical models of various organs and printing them. I think what we are trying to do a little bit different is print them but also make them active. We can print and then add on these actuators or embed so that they're dynamic and they're moving and tunable and controllable and can mimic disease.
Sally Kornbluth: Right. It's not the same as printing a static part. People are printing spine components, for example.
Ellen Roche: Exactly.
Sally Kornbluth: Turning a little bit to some of your personal questions. You grew up in Ireland, what was it like growing up there?
Ellen Roche: It was great. I was so lucky. Looking back, I think when you're a kid, you don't really appreciate it and take things for granted. I grew up in Galway, close to a place called Salthill, which is right on the ocean there and close to Galway City and walking distance from the university. It was really an ideal location to be close to all that. Went to school right beside the sea. I was thinking about it recently, during secondary school, which is equivalent to high school here, we would actually go and swim in the ocean on our lunch break and come back. It was a catholic school. We had uniforms and everything. They didn't really want us doing it, so we'd be putting on the uniforms over our wet, after the swim, trying to hide our hair dripping wet. That was great. It was a beautiful place to grow up, and close to Connemara. Like you mentioned, you can drive 20 minutes and you're in this very different landscape.
Sally Kornbluth: That's a beautiful area. As I mentioned before our conversation here, we were on vacation there and it was great. You wound up in a career far removed probably from what your childhood was like. What sort of experiences set you on this path?
Ellen Roche: My dad is a civil engineer and my mom passed away, but she was a radiographer and in the medical field, so I had both of those sides. My sister is a doctor. I considered medicine for a long time but really didn't want to give up the analytical, mathematical side of it. I ended up studying medicine for a while, but really to enhance my own research. I think as well, Galway is a hub for medical device companies. A lot of the larger multinational medical device companies set up in Galway for their manufacturing, and now their R&D is really strong there. Huge employer in Galway City. That influenced some of the courses in the university. The biomedical engineering degree was a four-year degree that was introduced just two years before I was choosing what I would study in undergrad. That was a great combination for me coming from high school. In Ireland, you decide when you're 17 or 18 what you're going to study straight away. I felt like that was a great combination. That allowed me then to do an internship in a company, which ended up being the one I worked with after graduation, which was just a great mix of the two. I think the university there and the research in that area has really grown. There's a good interaction between industry and academics there. That allowed me to have a stepping stone into industry in the U.S. and eventually academia in the U.S. as well.
Sally Kornbluth: That's great. What do you think you'd be doing then if you weren't doing this kind of work? Do you think you would've gone into medicine?
Ellen Roche: I think probably, yes. I really enjoyed it when I studied it. It's fascinating to learn about all the various aspects of medicine. I really enjoy the part of my job when I think about designing devices that can ultimately help patients and improve patient outcomes. I think I can do that in the job I'm in now, but if it wasn't this, I would probably be doing it in medicine.
Sally Kornbluth: What do you like to do outside of work?
Ellen Roche: At the moment, I am very busy with a young family. I have three daughters, they're two, five, and seven.
Sally Kornbluth: You have no free time.
Ellen Roche: I don't really have a whole lot of time for myself, but I enjoy bringing them to their activities and hanging out with them and spending time with them. They're great fun. I guess I have started to get back into doing some triathlons that I used to do when I was pre-kids. Just gradually getting back into that, which has been fun. I used to play traditional music as well when I was in school in Ireland. I haven't managed to do that for a while, but maybe soon.
Sally Kornbluth: Do you find that while you're practicing for your triathlon, you're running scientific ideas through your head?
Ellen Roche: Oh, yes, totally. Often I think when you're writing a proposal or thinking about how to frame something, you're writing at your desk, but if you go for a run or a swim, sometimes you can really clarify, "Oh, this is how I want to frame it."
Sally Kornbluth: If you're fit, so you don't have to concentrate on breathing. You can actually think about other things.
Ellen Roche: Right now, I do have to concentrate on breathing.
Sally Kornbluth: Anything you really want listeners to take away from your experience? In other words, if you were advising current students how to think about their futures, what sort of words of wisdom might you impart?
Ellen Roche: I often get questions from students who are considering whether to go an industry or academic route, and maybe decide between medical device engineering or medicine. I think my journey wasn't linear, really. I went from undergrad to industry in Ireland and the U.S. and then back to Ireland and then PhD much later. There was five years of industry in between, and then I studied medicine for a while and I did my PhD, and then a postdoc back in Ireland and then here. I think it's okay to take opportunities as they come up, as long as you're really passionate about what you do. Sometimes you go one route and it helps you to get to another one. It's not like it's a one-way and there's no return. There's really great ways now I think to combine some aspects of industry and academia. Whether your primary appointment is in an academic institution or industry, you can really collaborate a lot. There's loads of jobs at that intersection, too. The same with different fields of research, mechanical engineering versus bioengineering. I really enjoy being at the intersection of both. I think it's very daunting deciding which path to take, but I think there are always ways to figure out and to craft your own niche. Often it's at the intersection of many roles.
Sally Kornbluth: Right. I think some of the multidisciplinary work that you've described, in a way, required your non-linear journey.
Ellen Roche: Absolutely. Yes.
Sally Kornbluth: I think your point about following your passions is really important because I think when people do something, take a step because they think it's going to be good for them, or they think it's going to help their future work, you just don't know where things are going to go.
Ellen Roche: Exactly. Yes. I would never have guessed when I was in California that it would help me in a job as a professor at MIT. No way.
Sally Kornbluth: Exactly.
Ellen Roche: It really has helped a lot.
Sally Kornbluth: Exactly. I've really enjoyed our conversation.
Ellen Roche: Me, too. Thank you.
Sally Kornbluth: To our audience, I'd love to hear what you think of these podcasts, what you'd like to hear next. Send your suggestions to podcasts@mit.edu or message at @mit on any social media platform. I look forward to hearing from you. Thank you all again for listening to Curiosity Unbounded. I very much hope you'll join us again. I'm Sally Kornbluth. Stay curious.