Approximately 95 percent of cancer mortality is caused by metastasis. This fact is what motivates many cancer researchers to focus on finding new ways to stop or kill the growth of metastatic cancer cells. A new paper published in Nature Genetics focuses on research done to find out how cancers metastasize using new next-generation sequencing tools, specifically targeting endometrial cancer. The researchers performed whole-exome sequencing of 98 tumor biopsies and analyzed The Cancer Genome Atlas (TCGA) data to identify new recurrent alterations in primary tumors.
William Gibson, a first author of the paper and a current MD-PhD student in the Harvard-MIT Health Sciences and Technology program, explains that it is often difficult to obtain paired samples of primary and metastatic tumors: “One cohort of patients in whom you can obtain primary and metastatic tissue is in endometrial cancer patients for whom both the primary tumor and abdominal metastases are resected during the same operation. Additional research into endometrial cancer in particular is important as it is the second most common cause of gynecologic cancer mortality.” This led Gibson and his colleagues to focus on endometrial cancer for the study.
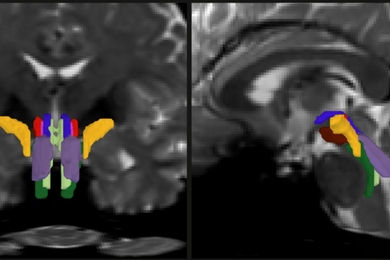
A mutation family tree
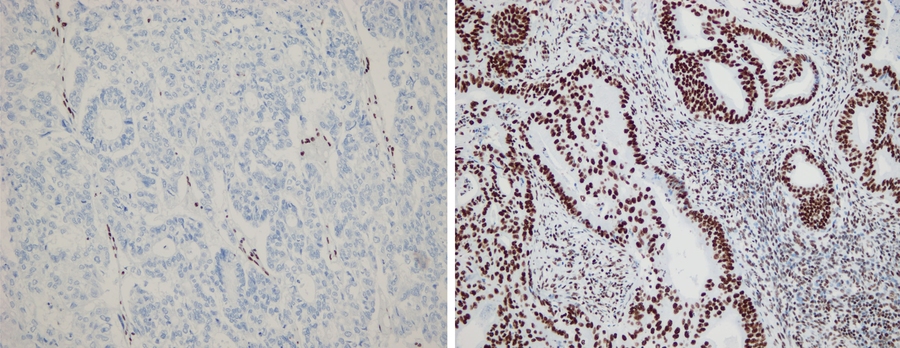
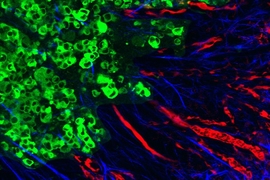
Each time a cancer cell acquires a new mutation, it passes the mutation on to all of its descendants. By finding the set of mutations in each metastasis, the researchers could create a family tree describing the evolutionary history of the cancer. They found that most metastases come from a single founding subpopulation of the primary tumor. When the researchers looked at the family trees describing the history of each tumor, they discovered that metastases had a significant tendency to cluster on one branch of the tree.
The researchers note that this fact alone doesn’t tell the whole story. It could be that these cells have acquired some special new abilities that allow them to repeatedly leave the primary tumor to establish metastatic colonies. Alternatively, it might be easier for cancer cells to metastasize once they have already done so.
Metastasis begets metastasis
In this model, the metastasis itself seeds the other metastases. The researchers weren’t able to distinguish these possibilities in the study. However, Gibson says, “Either way, we now know the cancer cells in these metastases aren’t there solely because they were lucky. We hope that we can replicate these findings in other tumor types.”
Gibson and his colleagues learned about some new driver genes that are mutated in endometrial cancer. “By changing the way we detected mutations in tumors with altered DNA repair, we were able to discover certain recurrent gene mutations. One of the genes most frequently mutated, NRIP1, is involved in the estrogen receptor pathway, which we are able to target with hormone therapy. It’s still unclear whether or not NRIP1 mutations will reveal a therapeutic vulnerability,” Gibson says.
The team sees this research impacting therapeutics in two ways:
First, the team found that certain common drive gene mutations actually occur late in cancer evolution. By sequencing multiple biopsies from the same individual, they were able to assess whether the mutations in driver genes were detected in all biopsies. For certain genes, like the epigenetic modifier ARID1A, mutations were frequently detected in only some biopsies. “This tells us that the cancer formed before it developed these mutations, and gives us reason to believe that not all of the cancer cells rely on this genetic alteration to stay alive. As such, therapies that aim at targeting ARID1A alterations may fail at a higher than expected rate. We are beginning to see which mutations help to initiate tumors and which mutations help tumors to progress,” Gibson explains.
Second, the new research suggests that there are unlikely to be any metastasis-specific driver genes that are recurrently mutated in the majority of metastases. There has previously been a hope that metastases might need to acquire some specific properties that allow them to execute the complex set of steps involved in metastasis.
“If this were the case,” Gibson says, “we could potentially design drugs that block these properties and prevent metastasis. We could not find any evidence of metastasis-specific driver genes and think it is unlikely that we will ever find genes like this in the majority of endometrial cancer metastases. Ultimately, these results tell us that to treat metastases, our best strategy is to refocus on genetic features common to all cells of the tumor.”
During the process of this paper’s publication, a senior author and member of the Norwegian group who has spent substantial time at the Broad Institute, Helga Salvesen, died unexpectedly during the revisions to the paper. The Broad will host a memorial symposium on endometrial cancer in her honor on October 24 from 8 a.m. to 5 p.m. For more information about the symposium, please contact SalvesenMemorial@broadinstitute.org.