Influenza viruses that emerge from birds or pigs can create pandemic flu if they gain the ability to spread from person to person. New research from MIT shows that two recently emerged bird flu strains, which do not spread easily now, could become much more infectious with just one or a few genetic mutations.
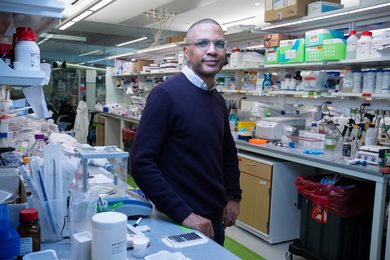
The studies, which focused on the H5N1 and H7N9 flu strains, should help public health officials monitor evolving flu viruses for potential human-to-human transmission. They could also guide the development of new vaccines, says Ram Sasisekharan, the Alfred H. Caspary Professor of Biological Engineering and senior author of two papers appearing in the June 6 online edition of the journal Cell.
Flu viruses are classified according to the type of hemagglutinin (HA) protein they contain; the strains that most commonly infect humans contain H1 or H3 proteins. However, other HA types can evolve to attack human respiratory cells, potentially posing a significant threat because human immune systems are often not prepared to fight them off.
Sasisekharan and his colleagues set out to characterize the H5N1 and H7N9 viruses’ ability to infect humans by analyzing the structure of their HA proteins. In previous studies, Sasisekharan has shown that whether a flu virus can infect humans depends on its HA protein, which binds to glycan or sugar receptors found on the surface of respiratory cells. These glycan receptors come in two shapes: one that resembles an umbrella, and another that resembles a cone. To infect humans, flu viruses must bind to the umbrella-shaped receptors.
So far, neither H5N1 nor H7N9 has been able to efficiently bind human glycan receptors.
H5N1
H5N1 leapt from birds to humans about 10 years ago; it has since infected nearly 600 people around the world, and about 60 percent of those infections have been fatal.
In the new Cell paper, the MIT team studied the structure of HA proteins from hundreds of H5N1 strains and identified three HA regions where one or two mutations would enable the HA to bind efficiently to human receptors. Most of these regions affect the base of the receptor-binding site.
The researchers also found that H5N1 has been evolving rapidly since 2005, but none of the current strains have all of the mutations needed to spread from human to human. However, the researchers found one strain that needs only a single amino-acid switch to become highly infectious, and several others that need only two. “There are multiple different ways that this can happen,” says Sasisekharan, who is also a member of MIT’s Koch Institute for Integrative Cancer Research.
Furthermore, because of all of the viral evolution that has occurred since 2005, the H5N1 vaccines that governments have stockpiled would probably no longer be effective, Sasisekharan says. “There is cause for concern,” he says. “Yet these findings open opportunities to make sure that some of these newer strains do become part of the stockpiling, because they are closer to human adaptation.”
H7N9
H7N9 has infected at least 132 people this year, mostly in China, and there have been 37 deaths, according to the World Health Organization — a lower fatality rate than that of the H5N1 virus.
The MIT researchers found that although the current circulating forms of H7N9 bind weakly to human receptors, a change in just one amino acid would dramatically increase the HA protein’s binding strength. “It was not a marginal increase; we saw a pretty significant increase in receptor binding,” Sasisekharan says. “Our research provides insights to help keep track of potentially important mutations so that proactive steps can be taken to be better prepared against dangerous viruses.”
H7 typically circulates only in nonhuman animals, so most people would not be able to mount much of an immune response against H7N9. There are some H7 vaccines now in development, but the strains being used to create those vaccines are so different from H7N9 that they would likely not offer any protection, Sasisekharan says.
The information provided by the two studies should have a direct impact on both influenza risk assessment and vaccine development, says Linfa Wang, director of the program in emerging infectious disease at the Duke-NUS Graduate Medical School in Singapore.
“Their unique approach, incorporating structural topology of the host receptor glycan bound to key viral surface protein (HA) and the inter-residue interaction network in the receptor binding site of HA, is extremely powerful in providing crucial information within a short time period,” says Wang, who was not part of the research team.
Lead author of the H5N1 paper is MIT research scientist Kannan Tharakaraman. Other authors are research scientist Rahul Raman, research affiliate Karthik Viswanathan, graduate student Nathan Stebbins, postdoc Akila Jayaraman, technical associate Arvind Krishnan and visiting scientist Viswanathan Sasisekharan.
Tharakaraman and Jayaraman are lead authors of the H7N9 paper. Raman, Viswanathan, Stebbins and Sasisekharan are also authors of that paper, along with technical associate David Johnson and research affiliate Zachary Shriver.
The research was funded by the National Institutes of Health and the Singapore-MIT Alliance for Research and Technology.
MIT studies of two influenza viruses reveal genetic mutations that could result in pandemic flu.
Publication Date:

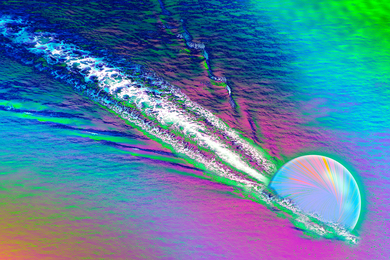
Caption:
MIT researchers focused two recent studies on the H5N1 and H7N9 (shown) flu strains.
Credits:
Image: Cynthia S. Goldsmith and Thomas Rowe/Centers for Disease Control and Prevention