Tissue engineering has long held promise for building new organs to replace damaged livers, blood vessels and other body parts. However, one major obstacle is getting cells grown in a lab dish to form 3-D shapes instead of flat layers.
Researchers at the MIT-Harvard Division of Health Sciences and Technology (HST) have come up with a new way to overcome that challenge, by encapsulating living cells in cubes and arranging them into 3-D structures, just as a child would construct buildings out of blocks.
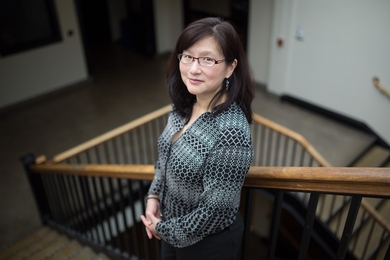
The new technique, dubbed “micromasonry,” employs a gel-like material that acts like concrete, binding the cell “bricks” together as it hardens. Ali Khademhosseini, assistant professor of HST, and former HST postdoctoral associate Javier Gomez Fernandez describe the work in a paper published online last week in the journal Advanced Materials.
The tiny cell bricks hold potential for building artificial tissue or other types of medical devices, says Jennifer Elisseeff, associate professor of biomedical engineering at Johns Hopkins University, who was not involved in the research. “They’re very elegant and have a lot of flexibility in how you grow them,” she says. “It’s very creative.”
Controlled structure
To obtain single cells for tissue engineering, researchers have to first break tissue apart, using enzymes that digest the extracellular material that normally holds cells together. However, once the cells are free, it’s difficult to assemble them into structures that mimic natural tissue microarchitecture.
Some scientists have successfully built simple tissues such as skin, cartilage or bladder on biodegradable foam scaffolds. “That works, but it often lacks a controlled microarchitecture,” says Khademhosseini, who is also an assistant professor at Brigham and Women’s Hospital. “You don’t get tissues with the same complexity as normal tissues.”
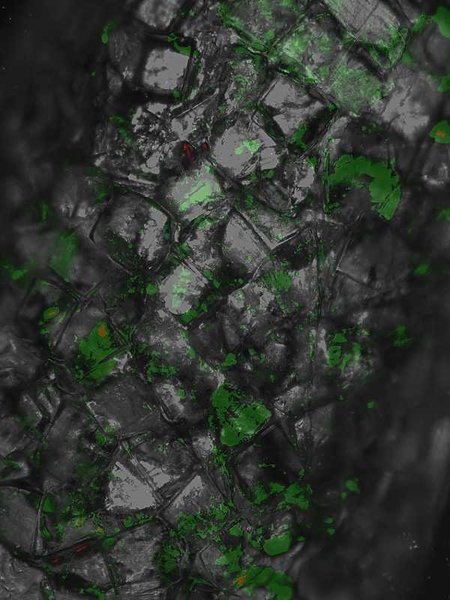
The HST researchers built their “biological Legos” by encapsulating cells within a polymer called polyethylene glycol (PEG), which has many medical uses. Their version of the polymer is a liquid that becomes a gel when illuminated, so when the PEG-coated cells are exposed to light, the polymer hardens and encases the cells in cubes with side lengths ranging from 100 to 500 millionths of a meter.
Once the cells are in cube form, they can be arranged in specific shapes using templates made of PDMS, a silicon-based polymer used in many medical devices. Both template and cell cubes are coated again with the PEG polymer, which acts as a glue that holds the cubes together as they pack themselves tightly onto the scaffold surface.
After the cubes are arranged properly, they are illuminated again, and the liquid holding the cubes together solidifies. When the template is removed, the cubes hold their new structure.
Gomez Fernandez and Khademhosseini used this method to build tubes that could function as capillaries, potentially helping to overcome one of the most persistent problems with engineered organs — lack of an immediate blood supply. “If you build an organ, but you can’t provide nutrients, it is going to die,” says Gomez Fernandez, now a postdoctoral fellow at Harvard. They hope their work could also lead to a new way to make artificial liver or cardiac tissue.
Other researchers have developed a technique called organ printing to create complex 3-D tissues, but that process requires a robotic machine that is not in widespread use. The new technique does not require any special equipment. “You can reproduce this in any lab,” says Gomez Fernandez. “It’s very simple.”
To get to the point where these engineered tissues could become clinically useful, “the short-term next step is really looking at different cell types and the viability of tissue growth,” says Elisseeff. The researchers are now doing that, and they are also exploring the use of different polymers that could replace PEG and offer more control over cell placement.
Researchers at the MIT-Harvard Division of Health Sciences and Technology (HST) have come up with a new way to overcome that challenge, by encapsulating living cells in cubes and arranging them into 3-D structures, just as a child would construct buildings out of blocks.
The new technique, dubbed “micromasonry,” employs a gel-like material that acts like concrete, binding the cell “bricks” together as it hardens. Ali Khademhosseini, assistant professor of HST, and former HST postdoctoral associate Javier Gomez Fernandez describe the work in a paper published online last week in the journal Advanced Materials.
The tiny cell bricks hold potential for building artificial tissue or other types of medical devices, says Jennifer Elisseeff, associate professor of biomedical engineering at Johns Hopkins University, who was not involved in the research. “They’re very elegant and have a lot of flexibility in how you grow them,” she says. “It’s very creative.”
Controlled structure
To obtain single cells for tissue engineering, researchers have to first break tissue apart, using enzymes that digest the extracellular material that normally holds cells together. However, once the cells are free, it’s difficult to assemble them into structures that mimic natural tissue microarchitecture.
Some scientists have successfully built simple tissues such as skin, cartilage or bladder on biodegradable foam scaffolds. “That works, but it often lacks a controlled microarchitecture,” says Khademhosseini, who is also an assistant professor at Brigham and Women’s Hospital. “You don’t get tissues with the same complexity as normal tissues.”
The HST researchers built their “biological Legos” by encapsulating cells within a polymer called polyethylene glycol (PEG), which has many medical uses. Their version of the polymer is a liquid that becomes a gel when illuminated, so when the PEG-coated cells are exposed to light, the polymer hardens and encases the cells in cubes with side lengths ranging from 100 to 500 millionths of a meter.
Once the cells are in cube form, they can be arranged in specific shapes using templates made of PDMS, a silicon-based polymer used in many medical devices. Both template and cell cubes are coated again with the PEG polymer, which acts as a glue that holds the cubes together as they pack themselves tightly onto the scaffold surface.
After the cubes are arranged properly, they are illuminated again, and the liquid holding the cubes together solidifies. When the template is removed, the cubes hold their new structure.
Gomez Fernandez and Khademhosseini used this method to build tubes that could function as capillaries, potentially helping to overcome one of the most persistent problems with engineered organs — lack of an immediate blood supply. “If you build an organ, but you can’t provide nutrients, it is going to die,” says Gomez Fernandez, now a postdoctoral fellow at Harvard. They hope their work could also lead to a new way to make artificial liver or cardiac tissue.
Other researchers have developed a technique called organ printing to create complex 3-D tissues, but that process requires a robotic machine that is not in widespread use. The new technique does not require any special equipment. “You can reproduce this in any lab,” says Gomez Fernandez. “It’s very simple.”
To get to the point where these engineered tissues could become clinically useful, “the short-term next step is really looking at different cell types and the viability of tissue growth,” says Elisseeff. The researchers are now doing that, and they are also exploring the use of different polymers that could replace PEG and offer more control over cell placement.