Shortly after taking a faculty position at MIT, Joel Dawson '96, SM '97 got together with his former music teacher, Elena Ruehr, for coffee. Ruehr, an MIT lecturer in music and theater arts, mentioned that her husband, a neurologist at Beth Israel, was looking for an engineer to help him with a device to measure muscle loss in patients with Lou Gehrig's Disease and other muscular ailments.
Dawson, who specializes in microchips for wireless communications, was intrigued by the chance to do something outside his normal focus — and something that might have a direct impact on improving people's lives.
"A lot of my lab's research is on microchips for wireless systems, and electronics for cell phones and base stations," says Dawson, an associate professor of electrical engineering. "Wireless communications have helped people, but here the sense of help is a little bit more direct."
Dawson assisted Ruehr's husband, Dr. Seward Rutkove, with a muscle probe that is now being tested in patients at Beth Israel Deaconess Medical Center, where Rutkove is director of the Division of Neuromuscular Disease. Rutkove launched the project nearly a decade ago, in hopes of creating an easy, accurate way to monitor muscle loss in patients with Lou Gehrig's Disease, also known as amyotrophic lateral sclerosis, or ALS. The disease attacks the motor neurons that control voluntary muscle movement, leading to muscle weakness and atrophy.
"Once somebody is diagnosed, we don't have a great way of tracking the progression of the disease," says Rutkove.
Monitoring muscle
There is currently no treatment for ALS, but being able to accurately measure the progression of muscle loss could help researchers evaluate the effectiveness of drugs in clinical trials. Measuring muscle loss can also help doctors determine whether patients with treatable conditions such as inflammatory muscle diseases and orthopedic injuries are responding to therapy.
Currently, muscle function is tested with electromyography, which requires a needle to be placed in the patient's muscle as the patient contracts it — a painful procedure.
Rutkove and Dawson's probe assesses muscle loss using electric impedance myography (EIM), which measures muscle's resistance to an electrical current by passing a small, non-painful amount of current though the muscle using two electrodes. Rutkove has found that testing this resistance, or impedance, in muscular atrophy patients over time gives an accurate picture of muscle loss or gain.
To gather useful data, however, impedance must be measured in several different directions across a muscle, which can be time-consuming.
"If you're going to use electrodes, you stick them on, do your measurement and then re-apply them in a different direction and do the measurement again," says Dawson. "If you're interested in more than two directions, you can see it's a long procedure."
Rutkove enlisted Dawson to package the EIM system into a handheld device that doctors or physical therapists could easily use in their clinics. The new device contains two concentric rings of electrodes, which can be selectively activated to produce measurements in different directions, eliminating the need to repeatedly attach and detach single electrodes.
The first generation of their device produced accurate measurements, but with its spiky electrodes protruding, was not patient-friendly. It was also too complicated for a non-engineer to use easily. "In principle, we could have stopped there. We were getting the data we wanted, but a physical therapist is not going to use something like this. It's too cumbersome," says Dawson.
Making the probe more user friendly was a process Dawson compared to Apple's design of the iPod and iPhone. "MP3 players had been around for a long time, but they didn't really take off until they were easy to use," he says. "The iPhone practically teaches you how to use it. As user interface goes, it's genius."
With help from MIT postdoctoral associate Hong Ma, the team made the probe smaller and easier to use, and built an electrode array with a flat surface instead of spikes, making it more comfortable for patients.
William David, a neurologist at Massachusetts General Hospital who is familiar with the project, says that such a probe has the potential to one day become the neurologist's equivalent of a stethoscope.
"If they can successfully develop a handheld probe that you simply place on a patient's skin, it could be a non-invasive and very speedy test to perform at the bedside, with no discomfort to the patient," he says.
Dawson and his colleagues describe the latest generation of the EIM probe in a paper they have submitted to the Annals of Biomedical Engineering. They presented the first generation probe at the IEEE International Engineering in Medicine and Biology Conference last year.
Once perfected, the device could be used not only to study ALS but also to help evaluate muscle health in patients with other disorders, such as muscular dystrophy.
Rutkove, who has filed a patent on the device, has also talked to NASA about the possibility of using the probes to measure muscle atrophy in astronauts undertaking a potential mission to Mars. During the six-month trip, astronauts would lose muscle mass due to the lack of gravity, but there's no easy way to measure just how much their strength would be affected. With the probe, the astronauts could evaluate whether they strong enough to open the hatch door, or perform other tasks requiring strength.
Rutkove said he expects the device could be ready for commercial production within two years and could possibly receive FDA approval another year after that.
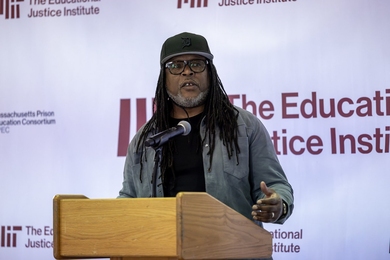
MIT engineer Joel Dawson and colleagues built a handheld probe that could help doctors monitor muscle atrophy in patients with Lou Gehrig's Disease and similar ailments.
Publication Date:

Caption:
Joel Dawson, associate professor of electrical engineering
Credits:
Photo: Patrick Gillooly

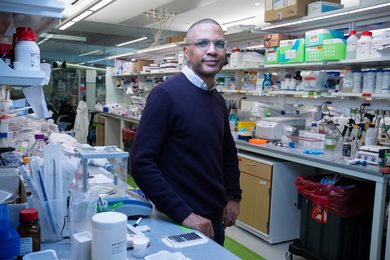
Caption:
Dawson holds up a prototype of a device to measure muscle loss in patients with Lou Gehrig's Disease and other muscular ailments.
Credits:
Photo: Patrick Gillooly