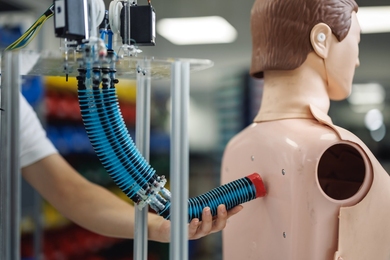
Researchers have been puzzled in recent years by observations that drug-releasing stents (mesh-like tubes implanted to hold patients' coronary arteries open) can increase the likelihood of blood clots and heart attacks. Now, a mathematical model developed by MIT engineers can predict whether particular types of stents are likely to cause life-threatening side effects.
The model "helps explain why some stents are better than others, and could predict which stents are predisposed to cause clotting," said Elazer Edelman, the Thomas D. and Virginia W. Cabot Professor of Health Science and Technology (HST) and senior author of a paper on the work appearing as the cover story of the Jan. 5 issue of the Journal of Controlled Release.
Edelman and HST postdoctoral associates Vijaya Kolachalama and Abraham Tzafriri designed the model to predict how the size and shape of a stent affects blood flow and drug distribution.
Drug-releasing stents are used in more than a million patients per year in the United States. The drugs, including paclitaxel and rapamycin, are intended to prevent tissue from growing inside the artery after it is inflated during angioplasty.
However, drug-releasing stents have been proven a "double-edged sword," Edelman said. The drugs successfully block tissue growth that could impede blood flow, but can have the unforeseen side effect of increasing the risk of blood clots and heart attacks.
This paper explains why: Stents affect the fluid dynamics of blood flowing past them and cause drugs to accumulate in certain areas. Too much drug buildup promotes clot formation.
The MIT model shows that the dynamics of blood flowing around a stent is similar to whitewater rapids, said Edelman. When water in a river flows over a boulder, some of the water strikes the base of the boulder, flies up in the air and comes back down, instead of flowing over the rock. This water continuously recirculates in the same area.
The same thing happens when blood flows across a stent: Drugs tend to accumulate and spin around in the recirculation zone. This is most likely to happen with stents that protrude further into the artery. "Until now, the degree to which recirculation zones impact the distribution of drugs was not appreciated," said Edelman.
This is the first time that a mathematical model has successfully predicted stent performance based on changes in arterial blood flow and design, and the researchers hope the model and concepts it establishes could aid efforts to design stents that allow drugs to be more evenly distributed throughout the area.
The model could also help the FDA in its approval processes, by helping regulators figure out which stents are most likely to be safe or harmful, based on their size and shape, which controls how they will affect blood flow.
Davis Arifin, a graduate student in the MIT-Singapore Alliance, is also an author of the paper.
This research was funded by the National Institutes of Health.
A version of this article appeared in MIT Tech Talk on January 14, 2009 (download PDF).