While it's not quite the fountain of youth, new medical developments at MIT do hold the promise of helping people age more gracefully and possibly live longer.
In recent years, MIT scientists have successfully grown "mini livers," thwarted coronary artery disease and retrained muscles to move after a stroke. "We are now at a watershed time when technology is about to burst forward. We need to learn how to use it," said Elazer R. Edelman, Herman Von Helmholtz Associate Professor in the Harvard/MIT Division of Health Sciences and Technology.
Professor Edelman, who has a background in medicine and engineering, uses mechanics and digital signal processing to study atherosclerosis (the progressive blockage of arteries) at the molecular level, and to engineer new ways to thwart it.
"Atherosclerosis is the leading cause of death and dying in western civilization," accounting for one million deaths and 2.75 million hospitalizations each year, he said. There are several causes of the disease, including infection, inflammation and excessive fat consumption.
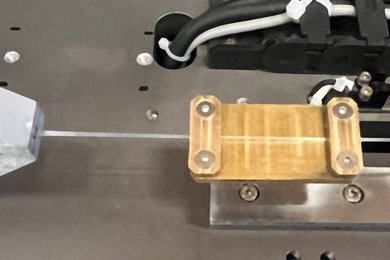
"Operations to deal with atherosclerosis are becoming increasingly sophisticated, but not increasingly successful," Professor Edelman said. Recent techniques include balloon angioplasty and the balloon-expandable vascular stent, a type of expanding mesh cylinder that can hold open and support a weak blood vessel. The balloon-expandable vascular stent was perfected in Professor Edelman's lab.
"These treatments work well, but only for a short period of time," he said. "We've delayed by three to nine months the inevitable progression of the disease, and have sometimes accelerated it." The stent, for example, may actually cause the removal of the endothelial cells that line blood vessels and help keep them strong. The removal of endothelial cells can cause infection and attract blockages.
Professor Edelman said his lab is looking at tissue engineering of endothelial cells using 3-D scaffoldings. A thin matrix of such engineered cells can essentially be wrapped around an artery, and the endothelial cells will actually diffuse into the blood vessel and repair it. He said such endothelial wraps currently are in Phase I clinical trials.
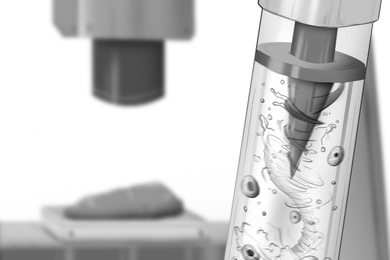
Linda G. Griffith, Karl Van Tassel Associate Professor of Chemical Engineering, also is engaged in tissue engineering using a biomaterial matrix to grow "mini livers." The research still is in development phase, but her laboratory has been able to grow rat liver tissue that appears to be similar in appearance to real liver tissue.
One key is to be able to use only small amounts of tissue donated by an individual patient to regrow large amounts of tissue on a complex biomaterial scaffold.
"We aim to make an 'organ' in vitro (outside the body)," said Professor Griffith. "There's a real shortage of donor organs, especially for pediatric livers, so for the past 15 years people have looked into taking a cell transplant approach to the liver." So far, Professor Griffith's lab has been able to grow liver cells, but not to the level of being transplantable.
Her research actually began with efforts to make an artificial ear for children either born without an ear lobe or who injured it after birth. She and her colleagues were able to devise an intricate biodegradable polymer scaffold using 3-D printing techniques to put cartilage cells onto the scaffold material. The cartilage cells grew to fill in the scaffold and form what looked like a human ear. The 3-D printing process, which builds up the polymer base and adds donor cells layer by layer, can be used to build up very fine internal structures as well.
Professor Griffith said the technology also is being applied to grow skin grafts using a small amount of donor material from patients with serious burns.
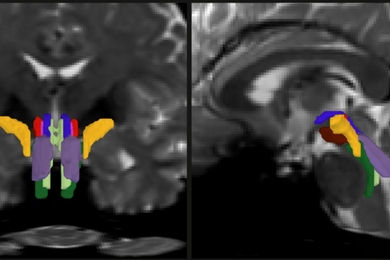
Professor Emilio Bizzi, head of the Department of Brain and Cognitive Sciences, is studying how the brain causes muscles to move, including how stroke victims can retrain their muscles even though cells critical to causing motion have been destroyed.
One of the discoveries in the past few years is that there are slight differences in the way in which cells are packed into areas of the brain's cortex and represent different functions, such as control of arms, legs, the neck and back muscles, he said.
"What happens when a stroke hits these areas? A lot of cells die, but there still are a lot of cells left," Professor Bizzi said.
Professor Bizzi is researching how cells that are not usually assigned to motor tasks can actually be recruited to make up the functions of cells that died during a stroke. "We're studying monkeys now to see which areas of the cortex are used to learn new tasks," he said. "We still need to know how the frontal lobe handles complex and simple movements."
A version of this article appeared in MIT Tech Talk on May 21, 1997.