A man with a history of cardiac arrhythmia is admitted to an emergency room in Virginia, with symptoms of chest pain and irregular heartbeat. Based on factors such as age, respiratory rate, blood pressure, and platelet count, doctors are able to determine the likelihood of his surviving under intensive care. They do this with the help of an intensive care unit (ICU) severity-of-illness score, the most common of which is the APACHE system. APACHE — Acute Physiology and Chronic Health Evaluation — was originally designed in the early 1980s as a tool for predicting, then presenting critical-care mortality risk in a simplified format.
With vital signs and serum levels checked, the man is estimated to have a 7 percent risk, suggesting a relatively low probability of dying during his ICU stay. The hospital will use this score to later assess its own performance, and compare similar patients’ outcomes with those of other hospitals.
Yet had the patient been Australian and brought to a critical care unit in Perth, the U.S.-centric APACHE score might have proven less useful, with his chances of survival a more complex matter, says Jesse Raffa, a research scientist at the Institute for Medical Engineering and Science (IMES) and lead developer of a new scoring system known as the Global Open Source Severity of Illness Score, or GOSSIS.
“It would be difficult to say if a model developed on American patients is relevant to such a patient in Australia,” Raffa says. “What we’re trying to do is come up with something more internationally appropriate.”
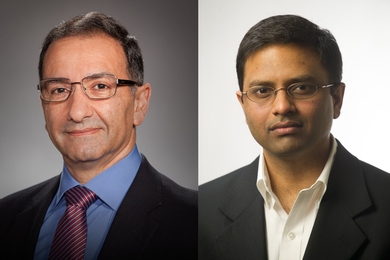
With GOSSIS, Raffa and a group of collaborators are looking to collect and incorporate hospital data from a range of countries, thus creating a truly universal ICU severity-of-illness score to be used in a variety of settings. Raff and the group — co-researchers Alistair Johnson, Tom Pollard, David Pilcher, and Omar Badawi, advised by Principal Research Scientist Leo Anthony Celi and part of the Laboratory for Computational Physiology, led by Professor Roger Mark at IMES, who along with participating hospitals are collectively titled the GOSSIS Consortium — aims also to provide a better calibrated system than older models. Initial funding for GOSSIS was provided by Philips Healthcare and the National Institutes of Health.
“APACHE’s primary use is for hospitals to monitor how well they’re doing,” Raffa says. “And calibration is important for benchmarking, or comparing survival statistics against those of other hospitals, and then assessing relative performance.”
While hospitals generally have an idea of their own patient mortality rates, Raffa says, well-calibrated prediction models are often lacking, making comparison to their peers difficult. “When you have a systematic approach — a validated algorithm — this leads to more accurate benchmarking of your center.”
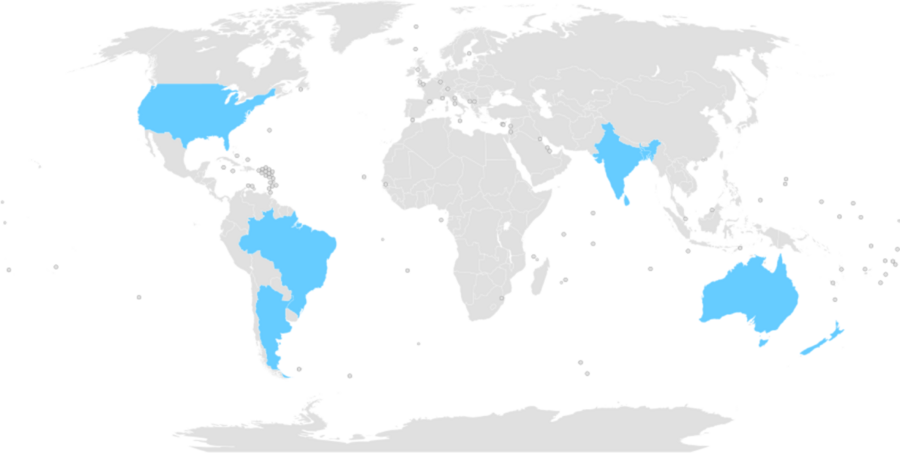
Nearly 45 U.S. hospitals currently contribute data to APACHE IV, a recent iteration of APACHE. In contrast, as of early 2019, GOSSIS-ready datasets exist for critical-care units in Argentina, Australia, New Zealand, Bangladesh, India, Nepal, Sri Lanka, Brazil, and 205 American hospitals. Combined with the international consortium members, the GOSSIS system will provide data from a total of more than 1,000 medical facilities.
An additional proposed benefit of GOSSIS: its cost-effectiveness. Unlike pricey APACHE scores, often challenging to obtain for hospitals with fewer resources and which cannot be considered fully analogous to reports from other countries, GOSSIS can be accessed, as well as added to, free of charge — a potential boon for the system, as with increased and more active participation, the algorithm itself has the unique opportunity to be regularly updated, and improved.
“GOSSIS is an important initiative for numerous reasons,” says Celi. “Foremost is its open-source nature, which allows for continuous evaluation and recalibration of the algorithm. This is difficult with proprietary scoring systems and would typically be accompanied by the vendors charging more for these services. The second reason is participation of a much larger number of countries that are traditionally left out from development of such scores. By having these countries contribute data to train the algorithm, it’s more likely that the algorithm will perform well on their population.”
Although GOSSIS will be available to any hospital seeking access, the researchers encourage as many intensive care units as possible, worldwide, to upload their data.
“By contributing their own critical care data, hospitals ensure they are well represented in the algorithm. Often hospitals are collecting all or part of these data elements anyway, particularly if they are using some other scoring system,” Raffa says.
He adds that homogeneity will not be a prerequisite for uploading data. “We recognize that not everyone will have perfect data, and we chose the approach we used with this in mind.”
Badawi, head of Health Data Science and AI at Philips Patient Care Analytics, is hopeful the system will have a major impact. “In 10 years’ time, we would envision a large consortium of data contributed from every region around the globe, which would enable for a variety of open source risk models to be available across countries.”
In its initial stages of adoption, GOSSIS is already gaining wide attention from the medical community. On Feb. 19, Raffa and his colleagues were accorded the Silver Medal Award for their work by the Society of Critical Care Medicine in San Diego. Reflecting on the award, Raffa says he was honored, especially as a data scientist, to be acknowledged by an organization of medical professionals.
“Having the team recognized with this award is an honor, and I think it illustrates well that data science, particularly when done collaboratively with clinicians, will have an important role in the future of clinical research,” Raffa says.
For more information and to become a part of the GOSSIS consortium, visit gossis.mit.edu.