Raise your hand if you are more afraid of the prospect of general anesthesia than of surgery itself. If you raised your hand, you are not alone, according to the newest faculty member at the Harvard-MIT Division of Health Sciences and Technology (HST).
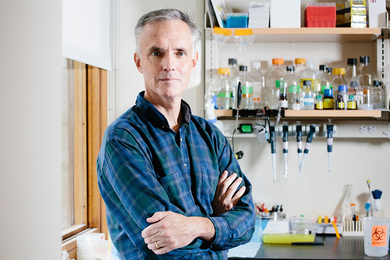
Dr. Emery N. Brown, who explores what happens to the brain during anesthesia, began a dual appointment as professor of health sciences and technology and professor of computational neuroscience in the Department of Brain and Cognitive Sciences (BCS) at MIT in October 2005.
"Anesthesia has taken on a mythical quality; it's not perceived as a neuro-physiological phenomenon," he said.
He describes the motivation behind his current research focus: "For many years, I was practicing anesthesiology, learning clinical skills in order to take care of patients, not thinking about how anesthesia affects patients. Then 10 years ago, when HST alum Dr. Greg Koski was the head of human studies at MGH, he said, 'It would be interesting to see an image, to see what happens when someone is under anesthesia.'" Brown was hooked.
"We say we induce anesthesia and then 'wake up' the patient," Brown said. "But in French the patient is r̩anim̩, or brought back to life. We haven't yet begun to think precisely about what we do, however. Anesthesia is not like sleep. It's not the same process."
Brown added, "Under anesthesia, one is insensitive to pain. If you were asleep, you would wake up if you had pain. Anesthesia has four aspects: loss of consciousness, analgesia, amnesia and loss of movement -- all while remaining hemodynamically stable, i.e., alive."
These are the basic principles behind Brown's investigation into what happens in the brain as it undergoes anesthesia and later is "reanimated."
"We have a vast array of questions," Brown said. "The way we give anesthesia now, it is a bit like dumping it into the whole brain so it acts everywhere in the brain. But if we can pinpoint the areas of the brain that are affected or need to be affected to free us from pain, we could conceivably think about designing a drug or a way to administer a drug that, for example, would not affect the respiratory system, that would allow us to lose consciousness of pain but still allow us to breathe."
His research team explores this by administering more and more of an anesthetic drug while measuring brain activity using MRI, fMRI and EEG simultaneously.
"We see how the regions of the brain stop talking to one another," he said. "We give subjects an auditory task -- they're asked to click a button with their left hand when they hear a low tone and click a button with their right hand when they hear a high tone -- in order to develop a clinical definition of anesthesia. When the subject stops responding we want to know what the EEG tells us and what the images show us."
One of Brown's collaborators is HST faculty member Dr. Richard Wurtman, professor of BCS and HST, who is looking for precise locations in the brain that are affected by anesthesia. Brown also collaborates with Matthew Wilson and HST-affiliated faculty member Christopher Moore, both of BCS, Nancy Kopell at Boston University, and Matti H��m��l��inen at HST's Martinos Center for Biomedical Imaging.
"Anesthesiology is being practiced today in much the same way it was when it was first developed at MGH 160 years ago (this October)," he said. "To me, anesthesiology is one of the most exciting frontiers in medicine. If you look at the deep question -- where did this person go under anesthesia -- we can get insights about consciousness, about sleep, about meditation. These are interesting, exciting medical and philosophical questions."
For more information, visit hst.mit.edu/images/upload/HST_Connector_Sum06.pdf.
A version of this article appeared in MIT Tech Talk on October 4, 2006 (download PDF).