CAMBRIDGE, Mass. -- MIT scientists, working in conjunction with researchers at Massachusetts General Hospital, have developed a non-invasive method of detecting early signs of cancer and heart attacks, Science magazine reported today.
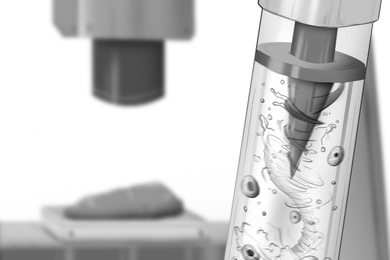
The new method is known as optical coherence tomography (OCT). OCT produces a clear picture of a cross-section of bodily tissue without requiring surgical biopsy. Using laser light, OCT can magnify tissue to allow visualization of individual cells without damaging the tissue.
OCT is based on optical fiber technology, the same technology now used in telecommunications. An optical fiber is a string-like component which guides light waves, allowing a light beam to be controlled over long distances and around bends.
OCT can be compared to ultrasound, except that infrared light waves are used rather than acoustic waves. Ultrasound sends out waves of sound and interprets the echoes reflected back by structures to create a visual image. A ship's sonar, for example, reveals the ragged terrain of the ocean far below it. Similarly, OCT shines a beam of infrared light into tissue structure, and its backreflections, measured from different positions, form an image of the terrain within. Thanks to OCT's high resolution -- ten times higher than either clinical MRI or high frequency ultrasound -- microscopic early signs of disruption in tissue terrain can be detected and treated.
The infrared light used in OCT is introduced to tissue by means of a small catheter, or endoscope, which can be used virtually anywhere in the body.
Seven authors are credited for the article in Science, titled, "In Vivo Endoscopic Optical Biopsy with Optical Coherence Tomography." They are senior author James G. Fujimoto, PhD., Professor in the Research Laboratory of Electronics (RLE) and in the Department of Electrical Engineering and Computer Science (EECS) at MIT, RLE postdoc Brett E. Bouma, and Guillermo J. Tearney, Stephen A. Boppart, and Costas Pitris, graduate students in EECS. Mr. Tearney is the first author cited. The second author cited, Dr. Mark E. Brezinski, is a cardiologist at Massachusetts General Hospital, an Assistant Professor at Harvard Medical School, and a Research Affiliate in the Research Laboratory of Electronics and in the Department of Electrical Engineering and Computer Science at MIT.
The program for developing OCT had two stages, the first of which involved imaging of transparent tissue. This began in 1991 in Professor Fujimoto's laboratory at MIT, in collaboration with Dr. Carmen A. Puliafito, Director of the New England Eye Center and Chairman of Ophthalmology at Tufts University School of Medicine. OCT imaging of the retina provides a "very powerful tool for ophthalmic diagnostics, especially for conditions such as glaucoma and macular edema," said Professor Fujimoto. To date, several thousand patients have been examined using OCT. The results suggest OCT may be a promising way to diagnose early-stage glaucoma.
In 1994, in a collaboration led by Professor Fujimoto and Dr. Brezinski, OCT imaging was developed for optical biopsy in nontransparent tissue, which represents most of the tissue of the body.
"The key advance described in the upcoming article in Science is the demonstration of OCT for imaging nontransparent tissue in vivo (in a living organism)," said Professor Fujimoto. In the article, the researchers used OCT to image the esophagus of a living rabbit. "This advance opens up the possibility of an incredibly broad range of clinical applications," added Professor Fujimoto.
Developing OCT to its current status required persistence and an effective collaboration among researchers.
"Three and a half years ago, I was told by many people that this project wouldn't work, that light wouldn't penetrate deeply enough. Now, we are just about ready to test OCT in patients through a high-speed, high-resolution catheter/endoscope-based system," said Dr. Brezinski.
"This could not have been accomplished by one or two individuals but represented the vertical integration of students, postdocs and investigators, a fact of which we are all very proud. If you compare this to other technologies like ultrasound and MRI, we have come a tremendous way in three and a half years," Dr. Brezinski added.
The researchers suggest that OCT will replace conventional biopsy for many applications in the future.
First, OCT can be used where conventional biopsy would be hazardous, with the brain and coronary arteries being the most prominent examples. Second, OCT could serve well where surgical biopsy misses the diagnosis, such as in early cancer detection in the colon, esophagus and cervix. Third, they suggest, OCT can be used to guide surgical and microsurgical procedures such as nerve repair or prostate surgery.
Further research with OCT includes working directly with patients; increasing the resolution to allow OCT to be applied to early diagnosis of such disorders as cervical cancer, and exploring technology to use with OCT, such as spectroscopy, which may allow biochemical as well as structural information to be gained from the tissue.
The National Institute of Health, the Office of Naval Research and the Whittaker Foundation provided funding for the research described in Science.