Using knowledge from several different fields, MIT scientists in the Harvard-MIT Division of Health Sciences and Technology have improved a method of delivering drugs directly to the site of heart bypass grafts or angioplastied vessels that may significantly reduce the relapse rate in patients who have had these procedures.
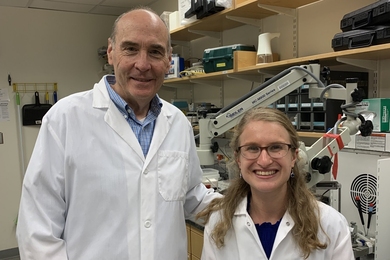
Dr. Aruna Nathan, a postdoctoral associate in biomedical engineering with Dr. Elazer Edelman of HST, summarized the work at a recent American Chemical Society meeting. Co-authors of the paper were Dr. Edelman and Mari Katada, a senior in mechanical engineering who assisted as a UROP student.
The perivascular drug delivery technology devised by Dr. Nathan and her colleagues involves implanting a pliable, gel-like sleeve around a blood vessel that is vulnerable to a repeat blockage. Embedded in the sleeve are tiny biodegradable polymer spheres (each several microns to several millimeters in diameter) containing a drug that seeps out as the spheres dissolve. Thus, the drug to prevent re-blockages can be delivered over a period of time to a specific site in the body without repeated surgical procedures.
Bypass operations and angioplasty (in which a balloon-tipped catheter is threaded through blood vessels to the heart and then inflated to compress a blockage, thus widening the vessel) are used to treat patients with atherosclerotic obstructions. However, 40 to 50 percent of these patients develop an accelerated form of the original disease, necessitating repeat procedures within just a few months, said Dr. Edelman, the Hermann von Helmholtz Assistant Professor of Health Sciences and Technology in the Harvard-MIT program. He is also a cardiologist at Brigham and Women's Hospital and an assistant professor at Harvard Medical School.
The rapid regrowth of the obstructions "is the limiting factor of everything we do that's good for the patients," he said. "If we can understand that process, we can halt it."
Dr. Edelman has been studying the process for eight years. The current work stemmed from a series of papers written by him in conjunction with Dr. Morris Karnovsky, Shattuck Professor of Pathological Anatomy at Harvard Medical School. Dr. Karnovsky had showed that angioplasty and blood vessel surgery have the side effect of blood vessel injury that can result in rapid growth of smooth muscle cells around the affected vessels. These cells normally constrict and dilate the vessels to regulate the rate of blood flow, but after surgery, they sometimes grow through the vessel wall, creating a new blockage.
Bypass and angioplasty procedures remove the endothelial cell lining of the blood vessel and in doing so, they also remove compounds produced by those cells that normally keep smooth muscle cell proliferation in check. At the same time, loss of the endothelial cells incites production of other factors that promote smooth muscle cell growth.
Dr. Karnovsky had earlier showed that endothelial cells produce a native form of the compound heparin to counteract growth of smooth muscle cells. He and his colleagues defined the physico-chemical properties of the native compound and processed heparin that make them potent anti-clotting agents as well as anti-proliferative compounds. They also showed how heparin could take the place of the native compound to control diseases of the blood vessel wall characterized by excessive smooth muscle cell growth.
In coordination with Dr. Edelman, he studied the optimum route of administration. Heparin cannot be taken by mouth without loss of its biological activity, but if injected, it can lead to serious systemic side effects. Relying on technology learned as a graduate student under the direction of Dr. Robert Langer, the Kenneth J. Germeshausen Professor of Chemical and Biomedical Engineering in the Department of Chemical Engineering at MIT (Tech Talk, April 6, 1994 and Oct. 15, 1993), Dr. Edelman sought to limit systemic effects by releasing the drug only outside the affected artery. Until recently, however, existing technology did not allow for precise regulation of the heparin release; Dr. Nathan addressed and solved this problem with her work.
Current studies focus on defining the ideal duration of drug administration. Researchers hope that a brief period of microspherical heparin release after surgery will permanently inhibit excessive smooth muscle cell growth.
The study of perivascular drug delivery is "multidisciplinary and multifaceted," bringing together fields including cell biology, materials science, mechanical engineering and vascular biology, Dr. Edelman noted. "In a sense, it's a secondary general science."
For instance, Dr. Nathan used her background in polymer chemistry and her more recently acquired knowledge of cell biology to determine the optimum physical and chemical properties for the drug delivery system. By changing the type of polymeric material used and the configuration of the release device (after considering alternatives such as slabs and sheets as matrices for the spheres), She was able to deliver substantially lower doses of heparin without loss of the desired effect.
Moreover, the devices degraded in the body without inducing an inflammatory response or injury of their own. Drs. Edelman and Nathan hope that further work refining the technology of localized drug delivery directly to blood vessels might provide added insight into the biology of vascular disease and potential alternative therapies for these illnesses.
If the technique is commercially developed, clinical trials could begin in a few years, Dr. Edelman said.
Support for the project is provided by the National Institutes of Health, the Whitaker Foundation for Biomedical Engineering, and Glycomed, Inc.
A version of this article appeared in the May 18, 1994 issue of MIT Tech Talk (Volume 38, Number 33).