An MIT scientist and colleagues report promising results in tests with mice of a novel vaccine delivery system that could eliminate several of the shots currently needed to immunize humans against diseases like tetanus and diphtheria.
Many people around the world still die of such diseases because they do not receive the full course of injections, so reducing the number of shots would save lives.
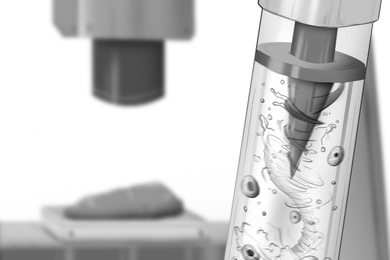
In the novel system, the vaccine is encapsulated in microscopic, biodegradable spheres that are injected into the body. As the microspheres break down, the vaccine is released. So "we're literally giving the equivalent of hundreds of little shots-maybe more-over time," said Robert S. Langer, Germeshausen Professor of Chemical and Biomedical Engineering in the Department of Chemical Engineering.
Present vaccines are injected in fluid form and degrade quickly. As a result, vaccination procedures for many diseases require multiple shots.
This summer Dr. Langer and colleagues reported results of the first tests in mice of a vaccine delivered in biodegradable microspheres. And those results support their theory that one injection of encapsulated vaccine could be as effective as many injections of a vaccine in fluid form.
In the work, which was published in the journal Pharmaceutical Research, the scientists found that mice injected with microspheres containing the tetanus vaccine showed an increased immune response to tetanus over time. In other words, they produced increasing amounts of antibody (the protein that attacks the tetanus pathogen). Mice injected with the regular fluid vaccine showed much less of an increase.
Currently the vaccination procedure for tetanus consists of three primary shots given during childhood, followed by a series of booster shots over a person's lifetime (adults who received primary shots as children need a booster every 10 years).
However, according to the World Health Organization "in many countries the dropout rates from individuals receiving a first dose but not successive doses can reach 70 percent," write Dr. Langer and colleagues in the Pharmaceutical Research article. One result: close to 700,000 newborns die of tetanus every year because women who have not been immunized properly can't pass on resistance to their babies.
The scientists don't know how many shots of fluid tetanus vaccine one dose of encapsulated vaccine might one day replace. But "I would be skeptical that we could provide lifelong immunity with a single shot," said George R. Siber, a scientist at the Massachusetts Public Health Biologic Laboratories and another author of the paper. "I think just getting it to take the place of the three primary shots would be great."
As reported in Pharmaceutical Research, the scientists developed many different formulations of microspheres to explore how different variables affect the release of vaccine over time. Such variables include the kind of polymer used to make the microspheres and the resulting microsphere size. Two formulations were selected for the mice studies; both resulted in significantly higher antibody levels than were obtained for the fluid vaccine.
According to Dr. Langer, however, "we don't yet know the optimal formulation" for encapsulated tetanus vaccine. To that end, scientists in Dr. Langer's laboratory are currently working on mathematical models that take into account the many interrelated variables that affect the release of vaccine. Such models, Dr. Langer said, "could someday lead to a recipe for the optimal [encapsulated] vaccine."
Ongoing work in Dr. Langer's laboratory also includes research on an encapsulated diphtheria vaccine, and the development of new microsphere polymers with properties that could lead to a vaccine with a "double hit," Dr. Langer said. These new polymers would "slowly release the vaccine and gradually break down into byproducts that stimulate the immune system to produce more antibodies."
Coauthors of the Pharmaceutical Research paper in addition to Dr. Langer and Dr. Siber are Rajesh Gupta of the Massachusetts Public Health Biologic Laboratories, Maria J. Alonso of the University of Santiago de Compostela in Spain, Smadar Cohen of Gurion University of the Negev in Israel, and Tae G. Park of Temple University in Philadelphia. Drs. Alonso, Cohen, and Park were all postdoctoral associates in Dr. Langer's laboratory at MIT when the studies reported in the Pharmaceutical Research paper were conducted.
The work, which was supported by grants from the World Health Organization and the National Institutes of Health, "really shows that it should be possible some day to develop practical, controlled-release vaccines," Dr. Langer concluded.
A version of this article appeared in the September 15, 1993 issue of MIT Tech Talk (Volume 38, Number 6).