MIT researchers reported at a March 23 American Physical Society news briefing that they have developed a new class of devices that can detect and image certain types of cancer before they are visible. Their method is as noninvasive as shining a tiny flashlight on the patient's tissue.
Rajan S. Gurjar, a postdoctoral associate who works with Professor of Physics Michael S. Feld, described the devices in a talk on March 24. One device is a simple portable machine that shines ordinary white light from a thin optical fiber probe, which is directed to the patient's tissue through an endoscope. This device analyzes tissue about 1 millimeter in diameter and has shown promising results in clinical studies. It accurately identified invisible precancerous changes in the colon and esophagus.
The second device, which has not yet been tested on patients, can map precancerous features over areas of tissue up to a few centimeters in diameter.
"These new methods, which can provide accurate results in a fraction of a second, may one day replace tissue biopsies in diagnosing certain types of cancers," Dr. Gurjar said.
Professor Feld predicted that in a couple of years, these devices will lead to a new class of endoscopes and other diagnostic instruments that will allow physicians to obtain high-resolution images. These easy-to-read images will map out normal, precancerous and cancerous tissue the way a contour map highlights elevations in reds, yellows and greens.
The effect was first realized by Vadim Backman, a graduate student in the Harvard-MIT Division of Health Sciences and Technology, and principal research scientist Lev Perelman, who were analyzing clinical data from the esophagus.
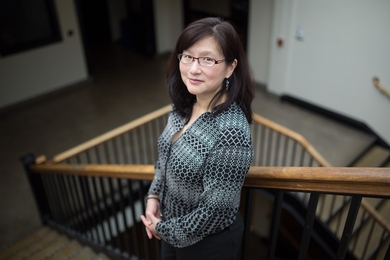
Both methods are based on a technique called light-scattering spectroscopy (LSS). LSS has been developed over the past two years at the MIT Laser Biomedical Research Center of the George R. Harrison Spectroscopy Laboratory, both directed by Professor Feld. The center, a National Institutes of Health resource for laser-related medical research, is at the forefront for research using light and spectroscopy for analyzing biological tissue.
CATCHING CANCERS EARLY
The LSS probe can be used on the epithelium -- the tissue lining cavities of the body such as the mouth, bladder and colon. Cancers that originate in the epithelium, which is often the body's first line of defense against invaders, include lung, stomach, breast and cervical cancer. Epithelial cancers can be treated successfully if caught early, but are difficult to detect because they are virtually invisible, even through an endoscope.
Dr. Jacques Van Dam, a gastroenterologist at Brigham and Women's Hospital in Boston, has worked with Professor Feld to test the LSS probe clinically. "Precancerous changes are not easily seen with the naked eye," he said. "If these very subtle changes are detected before they become cancerous, we can prevent cancer from forming."
Cancer develops through cell changes called dysplasia, which are currently detectable only through biopsies involving removal of tissue slices. "At the time of the biopsy, the physician can't see those changes. Being able to see the changes while actually there with the patient has not been possible before," Dr. Van Dam said.
"The ability to detect dysplasia eventually will have an impact on cancer treatment," he added. "There hasn't been anything like it before."
SHINING A LIGHT ON SPHERES
The LSS optical technique has long been used to study the size and shape of small spheres such as water droplets. For cancer detection, the method is applied to the cell's spheroid nucleus. Physics theory predicts that scattered light undergoes small but significant color variations when bouncing back from spheres of a certain size and refractive index.
Light is shined through the probe onto the patient's epithelial tissue. The probe collects the light that bounces back and analyzes its colors. The color content is then used to extract diagnostic information. Dr. Gurjar reported that in clinical tests, the probe accurately distinguished precancerous tissue in the colon and esophagus.
In the more advanced LSS imaging device that scans larger areas of tissue, a series of special light beams -- created from white light with colored filters and a polarizer -- are shined on the patient's epithelium. For each color of light, an electronic camera records a pair of images of the reflected light in two separate polarizations. The two images are then subtracted, which cuts out scattered background light and leaves behind only images relating to the cell nuclei.
The analysis can be done in a fraction of a second and the results displayed in a simple manner for the physician to interpret. "By analyzing the intensity variations in this back-scattered component from color to color, the nuclear size and density can be mapped," Professor Feld explained. Closely packed cells with larger-than-normal nuclei packed tightly with genetic material are markers of precancerous change.
"The images created with this new technique are different from ordinary microscopic images in that they provide hard-and-fast information about cellular features," he said. "We believe this is an important step that will lead to new optical tools for both early cancer diagnosis and developing a better understanding of how changes in the genetic material inside the cell's nucleus make the tissue more vulnerable to cancer."
A MORE ACCURATE READING
A condition called Barrett's esophagus provides an example of the limits of biopsy as a cancer detection method.
Barrett's esophagus is a reddening of the base of the esophagus caused by reflux, which is related to heartburn. Patients with Barrett's are more likely than the general population to develop cancer, so they are frequently tested for dysplasia.
Unfortunately, dysplasia in Barrett's is not visible through an endoscope, so biopsies are conducted randomly, leading to a large sampling error. In addition, dysplasia in Barrett's is difficult to diagnose. Experienced pathologists may disagree on biopsy results, and the stakes are high. If two pathologists agree that dysplasia is present, surgical removal of the esophagus is recommended.
"The excellent results of our clinical Barrett's esophagus study indicate great promise for LSS-based detection of dysplasia, which would be a big improvement in guiding biopsy and diagnosing dysplasia in the esophagus," Professor Feld said.
An interdisciplinary group of physicists, engineers, pathologists and clinicians participate in this ongoing research. Mr. Backman carried out experimental design and theoretical analysis. Other MIT participants include principal research scientists Perelman and Ramachandra Dasari.
Clinical work is conducted at Brigham and Women's Hospital and the West Roxbury Veterans Administration Hospital. The gastroenterologists are Dr. Van Dam, Dr. Steven Shields and Dr. Michael Wallace, now at the Medical University of South Carolina. The pathologists include Dr. James Crawford, now at the University of Florida; Dr. Maurice Seiler at the West Roxbury Veterans Administration Hospital; Dr. Maryann Fitzmaurice at University Hospitals of Cleveland; and Dr. Kamran Badizadegan at Children's Hospital in Boston.
This work is supported by the NIH.
A version of this article appeared in MIT Tech Talk on March 29, 2000.