Researchers led by Professor of Biology H. Robert Horvitz have found that a signaling protein that is part of a cell's natural suicide machinery may act as a "messenger of death" that travels to the cell's nucleus to execute the process of programmed cell death.
The finding adds an important piece to the puzzle of how malignant, malfunctioning or unneeded cells are instructed in apoptosis, or committing suicide, during an organism's development.
While the scientists emphasize that there is much more work to be done, they say that studies of the proteins that cause apoptosis might offer targets for drugs that can prevent cell death related to heart attacks, strokes or Alzheimer's disease. Led by Professor Horvitz, a Howard Hughes Medical Institute (HHMI) investigator, the research team reported their discovery in the February 25 issue of Science. The team also included scientists from the Max Planck Institute for Biological Chemistry in Germany and the Hebrew University in Jerusalem.
"Programmed cell death is a key mechanism for regulating cell numbers and connections and for sculpting tissues," said Professor Horvitz, who was among the pioneers in discovering the process. "Its misregulation can play a central role in certain cancers, autoimmune diseases and neurodegenerative diseases. We now know many of the molecules that control programmed cell death. Our new finding offers insights as to how one of these key molecules works."
The scientists conducted their research using the transparent nematode worm, Caenorhabditis elegans, long employed as a model to study apoptosis. The tiny worm contains exactly 1,090 cells, of which 131 undergo apoptosis, most during embryonic development.
Previous research by Professor Horvitz's team had shown that four proteins -- EGL-1, CED-9, CED-4 and CED-3 -- play a central role in the apoptotic machinery. CED stands for "cell death abnormal."
EGL-1 initiates apoptosis by inhibiting the normal restraining action of CED-9 on CED-4. Once unleashed from its restraints, CED-4 then triggers CED-3, which is a highly destructive protein-destroying enzyme that wreaks havoc on a cell's structures.
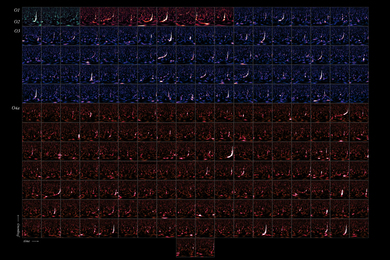
"Genetic studies of mutant worms that lacked one or another of these proteins had shown that they affected one another. We wanted to see whether and where they interact in the cell," said HHMI predoctoral fellow Bradley Hersh. Thus, said Hersh, he and his colleagues used antibodies that tagged each protein involved in apoptosis to reveal their cellular locations. Their experiments involved eliminating one or another of the signal proteins and studying the effects on protein localization.
"Our initial experiments showed that both CED-9 and CED-4 are localized to mitochondria," said Mr. Hersh. Mitochondria are the energy-producing powerhouses of the cell. Some scientists believe that mitochondria are the natural centers for the "sensors" that trigger programmed cell death, since malfunctioning mitochondria seriously compromise cell viability.
"Once we knew where these two proteins reside normally, the natural thing to do was look at how they affected the localization of one another," Mr. Hersh said. "We were surprised to find that that when we eliminated CED-9, CED-4 localization changed to the nucleus. After all, the mammalian counterpart of CED-4 is found mainly in the cytoplasm, and there was no indication that it would go to the membrane surrounding the nucleus."
Still mysterious, say Professor Horvitz and Mr. Hersh, is how CED-4 reaches the nuclear membrane. They are studying CED-4 mutants that fail to reach the nucleus. Such mutants might reveal clues to the transport process and its importance in cell death.
While the discovery of CED-4's translocation to the nuclear membrane is a basic one, it could have eventual clinical implications, said Mr. Hersh.
"If CED-4 translocation is required for activation, then inhibiting the translocation of a human counterpart of CED-4 might block cell death in such cases as ischemic injury in heart attacks or strokes," he said. "Also, in Alzheimer's disease, apoptosis may be central to the death of neurons, and blocking such a CED-4-like molecule might preserve brain tissue."
However, he continued, "we still don't know enough about this process to know whether inhibiting a CED-4-like protein, or translocation in the cell, will be possible. At this point, inhibiting human CED-3 counterparts, known as caspases, seems the most promising approach to blocking apoptosis, since these caspases have an established biochemical activity for which inhibitors have already been identified."
A version of this article appeared in MIT Tech Talk on March 8, 2000.