Scientists have made a major step toward finding a new class of oral drugs to treat HIV infection. They have identified a class of compounds that prevent HIV infection by stopping the virus at its port of entry into the cell.
Unlike currently used drugs that target HIV at other points during its life cycle -- after it has already infected the cell -- these compounds lock into a vulnerable "pocket" in the HIV's coat protein, preventing its fusion with cell membranes and thereby its ability to enter and infect cells.
The study was reported in the October 1 issue of Cell and was led by Professor of Biology Peter S. Kim, an affiliate of the Whitehead Institute for Biomedical Research and the Howard Hughes Medical Institute.
To identify these compounds, the scientists first designed a fragment of HIV coat protein such that its vulnerable pocket was properly displayed. The pocket was first identified two years ago by the Kim lab as being a potential drug target. But until now, researchers had been unable to recreate the pocket in the laboratory. In this study, the scientists not only recreated the pocket but also identified compounds that bind to it, and showed that the binding of the compound to the pocket prevents HIV from infecting cells.
Their findings hold great promise for identifying a new class of oral drugs for HIV infection and AIDS.
"The compounds that we identified can serve as leads, or starting points, for the development of small-molecule drugs that stop HIV entry into cells," said Professor Kim. "Alternately, scientists can use our 'pocket' to carry out high-throughput screening to identify other pocket-binding molecules. Finally, researchers can also identify new candidate drugs by their ability to disrupt the interaction between the pocket and the pocket-binding molecules."
To this end, and to speed up the process of finding new drugs, the Whitehead Institute will offer nonexclusive licenses of this technology to pharmaceutical and biotech companies worldwide.
The HIV pocket is small enough to be blocked by a drug of low molecular weight -- that is, a drug that can be taken orally. Also, the molecular architecture of this pocket is similar among different HIV strains, which means that drugs targeted at this pocket will be effective against various HIV strains, decreasing the likelihood that drug-resistant strains will emerge.
Scientists still need to do a lot of work before the compounds isolated in this study can become viable drugs, but "we hope that our X-ray structure [of the inhibitor bound to the HIV pocket] will assist such efforts," said Professor Kim.
COAT PROTEIN RESEARCH
The report is the culmination of decades long research into the structure of the HIV coat protein, called gp41. This protein plays a key role in allowing the virus to fuse with cells.
Scientists have long targeted gp41, hoping that a drug aimed at this protein could nip HIV infection in the bud by preventing the virus's ability to enter cells. Two years ago, Dr. Kim's lab at the Whitehead Institute used X-ray crystallography to decipher the structural architecture of the gp41 protein. When they looked at the striking images of this coat protein, they found that hidden within its intricately coiled-coil structure was a vulnerable cavity, a pocket that looked like an attractive drug target.
The discovery of this drug target was greeted with much excitement in the AIDS research community, but doubts remained about the potential to actually develop drugs for patients. Part of the skepticism stemmed from the fact that no one knew whether binding to this pocket by itself could inhibit HIV infection, and answering this question was not easy.
"Identifying molecules that bind this pocket was problematic because this region is only transiently exposed during the viral process, and the corresponding peptide fragments of gp41 aggregate," said Debra Eckert, a biology graduate student in the Kim lab and first author on the paper. "As a result, scientists had a hard time creating a stable structure of the HIV protein with this pocket exposed."
To use a motion picture analogy, although researchers could see the virus' Achilles heel in the movie, they found it hard to freeze the exact frame showing the virus's vulnerable pocket. And that in turn made it hard to identify drugs (or even test molecules) against this target.
In this study, scientists in the Kim lab reported that they found a creative way around this problem and designed a fragment of the HIV coat protein that correctly presents this pocket. The lab then used a technology called mirror-image phage display to identify a class of compounds that fit the pocket.
The technology takes advantage of the fact that all proteins and enzymes can exist in two mirror-image forms. Proteins that occur in nature are made out of so-called L-amino acids. Their synthetic alter personalities, made out of oppositely configured D-amino acids, are exact mirror images of the natural forms and have the opposite orientation.
The L- and the D- forms are like a pair of baseball gloves -- with identical catching abilities but opposite handedness. However, the D-forms are different from the naturally occurring L-forms in one key respect: while the L-forms are degraded by digestive enzymes and elicit a vigorous response from the immune system -- which makes them poor drug candidates -- the D-form is neither biodegraded nor processed by the human immune system. Peptides that are not degraded can turn out to be useful drugs; cyclosporin, a drug used to suppress the immune systems of kidney transplant patients, is one example.
"Our approach was to take advantage of these mirror-image properties to find D-peptides that bind to the HIV pocket," said Ms. Eckert. Once scientists found a class of D-peptides that bound to the pocket, they used X-ray crystallography to show that these molecules bind to the pocket only (and not other regions of the HIV protein) and that the binding inhibits HIV infection.
"Our finding that a molecule that binds solely to the HIV pocket is capable of inhibiting HIV infection provides proof of principle that pocket-binding molecules can stop HIV entry," said Professor Kim. The ability to prevent infection by binding solely to the pocket is important for developing oral drugs.
ATTRACTIVE DRUG BASIS
Physicians and patients prefer drugs administered orally. But finding them can be difficult because oral drugs generally have to be of low molecular weight (less than 1000 Daltons). The pocket identified by the Kim group is attractive because it is small enough that a drug with small molecular weight of about 500 Daltons would be sufficient to block its activity.
Another attractive feature of this HIV pocket is that it is highly conserved among different HIV strains and a drug targeted against this pocket would be effective against various strains, decreasing the likelihood of strains resistant to the drug emerging. Although the currently used combination therapies are successful, public health officials are increasingly seeing strains with resistance to these drugs. Having a third line of attack against this deadly virus would be a major advantage, said Professor Kim.
Drugs currently used to treat HIV infection fall into two categories: protease inhibitors that inhibit a protein called the HIV protease, and reverse transcriptase inhibitors, such as AZT, that target the HIV reverse transcriptase. Both drugs act after the virus has already infected cells; they prevent the infected cells from creating more HIV particles.
Scientists have long studied the viability of entry inhibitors -- synthetic peptides designed against the HIV coat protein -- to treat HIV infection. Many studies have been published showing that these peptides are effective in inhibiting HIV infection in cell cultures. In fact, one peptide called T-20 has shown antiviral effects in Phase I clinical trials. However, the problem is that because these are of high molecular weight (about 4,000 Daltons), they need to be injected into patients. Also, megadoses of these drugs are needed to achieve the antiviral effects.
"We hope that our technology will enable scientists to find a drug that has many of the attractive characteristics we seek in an anti-HIV drug -- orally bioavailable and targeting the virus before it even has a chance to infect cells." said Professor Kim.
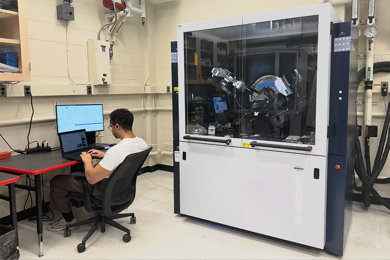
This research was funded by the National Institutes of Health and used the W.M. Keck Foundation X-ray Crystallography Facility at the Whitehead Institute and the Howard Hughes Medical Institute beamline at the National Synchrotron Light Source at the Brookhaven National Laboratory.
In addition to Professor Kim and Ms. Eckert, authors of the paper are research specialist Vladimir N. Malashkevich, technical assistant Lily H. Hong (SB 1999) and research associate Peter A. Carr.
A version of this article appeared in MIT Tech Talk on October 6, 1999.