In work that could lead to new treatments for atherosclerosis, the leading cause of death in Western industrialized countries, MIT biologists have nailed down the function of a key protein involved in cells' uptake of the so-called "good" cholesterol.
"This protein could be an attractive target for therapeutic intervention to manipulate levels of 'good' cholesterol in the blood," said Monty Krieger, professor of molecular genetics in the Department of Biology, who led the work. He noted that currently it's very hard to modify levels of this kind of cholesterol -- high-density lipoprotein (HDL) cholesterol -- in humans. Doing so could be beneficial because higher amounts are associated with a reduced risk of atherosclerosis.
Over the past two years, Professor Krieger and colleagues have reported indirect evidence for a role of this protein, a cell surface receptor, in HDL metabolism. The new work, however, is the first direct evidence. "It's the smoking gun that proves that this is a physiologically important receptor for HDL cholesterol," he said.
The research, which was conducted with mice, was reported in the November 11 Proceedings of the National Academy of Sciences. Professor Krieger also presented the findings at the annual meeting of the American Heart Association in Orlando, FL, on November 10.
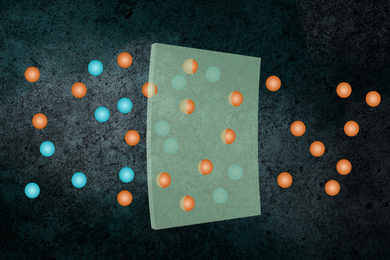
Atherosclerosis is characterized by the buildup of cholesterol in the walls of arteries. Clogged arteries, in turn, are a signature of coronary heart disease. The risk of developing atherosclerosis depends in large measure on the relative amounts of two particles that carry cholesterol through the bloodstream.
One, low-density lipoprotein (LDL), is known as "bad cholesterol" because higher levels are associated with an increased risk for atherosclerosis. The other, HDL, is called "good cholesterol" because high amounts are associated with a reduced risk for the disease.
But while a great deal is known about LDL and its receptor -- pivotal work on this earned Michael Brown and Joseph Goldstein a Nobel Prize in 1985 -- HDL has been slower to yield its secrets. Scientists believe that HDL extracts cholesterol from a variety of cells (including those in atherosclerotic plaques) and then carries it either directly or indirectly to the liver and to certain other tissues, where it is used to produce steroid hormones. One key to that process is an HDL receptor on the surface of cells at the end of the journey.
While such a receptor was identified for LDL two decades ago, an HDL counterpart was elusive -- until about two years ago. That's when Professor Krieger and colleagues first reported evidence that a protein they called "SR-BI" might be such a receptor. Key collaborators in this work included Susan Acton and Attilio Rigotti, postdoctoral students with Professor Krieger at MIT, and Kathy Landschultz and Helen Hobbs at the University of Texas Southwestern Medical Center (UTSMC).
Since then, Professor Krieger's group at MIT, sometimes in collaboration with other research teams across the country, has been exploring the structure and function of SR-BI. The leaders of some of these other teams include Helen Hobbs and Richard G.W. Anderson at UTSMC, David L. Williams at the State University of New York at Stony Brook, Vasillis I. Zannis at Boston University Medical Center, Karen F. Kozarsky at the University of Pennsylvania Medical Center, and Elazer R. Edelman and Robert Rosenberg at MIT and Harvard Medical School.
The current work "confirms the initial hypothesis regarding SR-BI function," Professor Krieger said. "Knockout" mice lacking the gene for SR-BI were found to have double the normal amount of HDL cholesterol in their blood. Without the receptor, the cholesterol couldn't be transferred normally into the liver and other cells that usually consume the material.
The HDL particles themselves were larger "because they were carrying more cholesterol. They couldn't efficiently get rid of their loads," Professor Krieger said. Finally, the knockout mice had "a dramatic reduction in the cholesterol content of their adrenal glands," a known repository for the material under normal conditions.
"The knockout mice prove that SR-BI plays a key role in determining HDL cholesterol levels and in delivering cholesterol to steroidogenic [steroid-producing] tissues like the adrenal gland," Professor Krieger concluded. He said that his team and other researchers expect that the receptor will have similar functions in humans.
Professor Krieger noted that prior to his team's work on SR-BI, many other researchers had made important contributions to the understanding of HDL metabolism in the blood and have pointed the way toward describing cellular HDL metabolism. However, he said, "the analysis of SR-BI has provided the first molecular handle for elucidating the mechanisms underlying cellular HDL metabolism."
What's next? For one, the researchers want to explore the role of SR-BI in the development of atherosclerosis, trying to learn whether there is a relationship between SR-BI activity and onset of the disease. They also hope to work out the molecular details of SR-BI-mediated HDL metabolism. The pathway by which the receptor retrieves cholesterol from HDL and deposits it into cells is "extremely ill-defined," Professor Krieger said.
Professor Krieger has been studying cholesterol and how it moves around the body for many years. The discovery of the HDL receptor, however, was serendipitous. "We were working on a completely different project which had nothing to do with HDL," he explained. "In that work, every time we did an experiment we found something totally unexpected." Most unexpected of all: the discovery of the long-sought HDL receptor.
Professor Krieger's collaborators on the PNAS paper are postdoctoral fellows Attilio Rigotti and Bernardo L. Trigatti, technical associate Marsha L. Penman, and research scientist Helen B. Rayburn, all of the MIT Department of Biology, and Joachim Herz of UTSMC.
The work was supported by the National Heart, Lung, and Blood Institute through its Program of Excellence in Molecular Biology. Dr. Rigotti was a Howard Hughes Medical Institute Postdoctoral Fellow, Dr. Trigatti was a Medical Research Council of Canada Postdoctoral Fellow, and Dr. Herz was the recipient of an Established Investigator Award from the American Heart Association and Parke-Davis.
A version of this article appeared in MIT Tech Talk on November 12, 1997.