A signaling protein known as STING is a critical player in the human immune system, detecting signs of danger within cells and then activating a variety of defense mechanisms.
STING is primarily on the lookout for DNA, which can indicate either a foreign invader such as a virus or damage to the host tissue or cell. When STING detects that danger signal, it can turn on at least three different pathways — one leading to interferon production, one to non-canonical autophagy (involved in recycling cell components and clearing pathogens), and a third to formation of the inflammasome, a complex of proteins that activates inflammatory responses. The mechanism by which STING stimulates interferon production is well characterized, but it has not been understood how it activates the other two processes.
Now, a team of MIT and Harvard Medical School researchers has discovered how STING activates those two pathways. They found that STING has a surprising and previously unknown function: It can act as an ion channel that allows protons to leak out of an organelle known as the Golgi body. This makes it the first human immune sensor that can translate danger signals into ion flow.
“Arriving at this new idea that STING is a proton channel required connecting prior findings by other labs that either STING or proton flux could activate the inflammasome and non-canonical autophagy, which led us to hypothesize that STING initiates or mediates proton flux to trigger both downstream processes,” says Nir Hacohen, a member of the Broad Institute of MIT and Harvard, a professor of medicine at Massachusetts General Hospital and Harvard Medical School, and a senior author of the study.
“Because of its importance to host immunity, there is a great interest in developing drugs that can activate or suppress STING activity, and the discovery of STING’s ion channel activity will provide new ways to think about designing therapeutics to modulate STING,” says Darrell Irvine, the Underwood-Prescott Professor at MIT with appointments in the departments of Biological Engineering and of Materials Science and Engineering; a member of MIT’s Koch Institute for Integrative Cancer Research and the Ragon Institute of MGH, MIT, and Harvard; and a senior author of the study.
MIT biology PhD student Bingxu Liu and Rebecca Carlson PhD ’23, a recent graduate of the Medical Engineering and Medical Physics program through the Harvard-MIT Division of Health Sciences and Technology, are the lead authors of the paper, which appears today in Science. Paul Blainey, the Karl Van Tassel Associate Professor of Biological Engineering at MIT and a member of the Broad Institute and the Koch Institute, is also an author of the paper.
A surprising role
STING (short for stimulator of interferon genes) is considered one of the major factors that triggers the immune response in the context of infection, autoimmunity, and cancer. Drugs that activate STING have been developed and tested in clinical trials as cancer immunotherapy drugs that would help stimulate the immune system to destroy tumors.
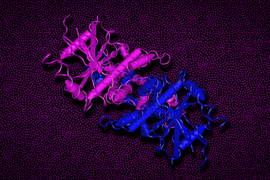
STING is a protein that can span membranes, and it is usually found embedded in the membrane of an organelle called the endoplasmic reticulum (ER). Once it detects DNA, it relocates to the Golgi body, where it begins to activate proteins that turn on genes required for interferon production.
“People know pretty well how STING induces interferon, but how STING induces autophagy and inflammasome formation has been an open debate in the field for the last 10 years,” Liu says.
Previous research has shown that both autophagy and formation of inflammasomes (large protein complexes that stimulate inflammation) can be provoked by protons leaking from cell organelles, which makes the inside of the cell more acidic. Because of that, the researchers wondered if STING might somehow induce proton leakage.
To explore this possibility, the researchers labeled the Golgi with a protein that fluoresces when the pH goes up. When they treated the cells with a molecule that activates STING, the Golgi became less acidic, meaning that it was losing protons. A genetic screen minimized the possibility of another ion channel controlling this ion flow, so the researchers hypothesized that STING itself was acting as a proton channel.
“In addition to its biological significance, this study is a notable example of the maturing functional genomics field, where pooled screening data are sufficiently reliable to set the direction of focused investigation — even from negative results, as was the case here,” Blainey says.
After running the structure of the STING protein through a computer model that can predict whether a given protein structure might contain a pore, the researchers found that the STING protein is predicted to contain a region that resembles a pore. Serendipitously, last year a company that was seeking STING agonists (molecules that activate STING) found a new molecule that was later shown by an academic group to bind in this precise location.
The MIT/Harvard team hypothesized that the agonist, known as C53, blocks the putative pore. When C53 was added to cells, protons did not leak out of the Golgi, and downstream pathways activating autophagy and inflammasome formation were not turned on, even if STING was activated through other means. However, interferon activation, which goes through a different pathway, still occurred.
“For the first time, we were able to decouple these downstream processes, where we can activate interferon with C53, but inhibit those other two pathways leading to autophagy and inflammasome formation,” Carlson says. “In the context of inflammatory diseases where STING is overactivated, we can now start asking which of those molecular mechanisms is most important and contributes the most to the phenotype that we’re seeing.”
Selective control
In future studies, the researchers hope to use C53 to determine the relative importance of these three pathways and try to figure out which ones would be most useful to stimulate or to block to treat a variety of diseases.
The U.S. Food and Drug Administration has not approved any STING agonist thus far, although multiple clinical trials are currently underway. One potential reason that other STING agonists have not made it beyond clinical trials is that the treatment can result in unwanted cell death mediated by STING. Drugs that stimulate interferon production but not cell death or other inflammatory pathways could offer a way to overcome that obstacle, according to the MIT/Harvard team.
The researchers hope to explore whether STING might play a role in influencing the behavior of other cellular activities known to be controlled by ion channels. “Now that we know that STING is an ion channel, we can propose other effects that we think could occur based on this knowledge that STING does transport protons,” Carlson says.
The research was funded by the U.S. National Institutes of Health, the Howard Hughes Medical Institute, a Fannie and John Hertz Foundation Fellowship, a U.S. National Science Foundation Graduate Research Fellowship, a European Molecular Biology Organization Fellowship, and a Cancer Research Institute/Bristol Myers Squibb Fellowship.