Scientists are catching up to what parents and other caregivers have been reporting for many years: When some people with autism spectrum disorders experience an infection that sparks a fever, their autism-related symptoms seem to improve.
With a pair of new grants from The Marcus Foundation, scientists at MIT and Harvard Medical School hope to explain how this happens in an effort to eventually develop therapies that mimic the “fever effect” to similarly improve symptoms.
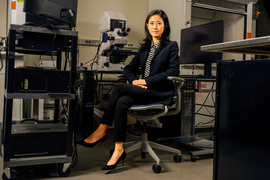
“Although it isn’t actually triggered by the fever, per se, the ‘fever effect’ is real, and it provides us with an opportunity to develop therapies to mitigate symptoms of autism spectrum disorders,” says neuroscientist Gloria Choi, associate professor in the MIT Department of Brain and Cognitive Sciences and affiliate of The Picower Institute for Learning and Memory.
Choi will collaborate on the project with Jun Huh, associate professor of immunology at Harvard Medical School. Together the grants to the two institutions provide $2.1 million over three years.
“To the best of my knowledge, the ‘fever effect’ is perhaps the only natural phenomenon in which developmentally determined autism symptoms improve significantly, albeit temporarily,” Huh says. “Our goal is to learn how and why this happens at the levels of cells and molecules, to identify immunological drivers, and produce persistent effects that benefit a broad group of individuals with autism.”
The Marcus Foundation has been involved in autism work for over 30 years, helping to develop the field and addressing everything from awareness to treatment to new diagnostic devices.
“I have long been interested in novel approaches to treating and lessening autism symptoms, and doctors Choi and Huh have honed in on a bold theory,” says Bernie Marcus, founder and chair of The Marcus Foundation. “It is my hope that this Marcus Foundation Medical Research Award helps their theory come to fruition and ultimately helps improve the lives of children with autism and their families.”
Brain-immune interplay
For a decade, Huh and Choi have been investigating the connection between infection and autism. Their studies suggest that the beneficial effects associated with fever may arise from molecular changes in the immune system during infection, rather than on the elevation of body temperature, per se.
Their work in mice has shown that maternal infection during pregnancy, modulated by the composition of the mother’s microbiome, can lead to neurodevelopmental abnormalities in the offspring that result in autism-like symptoms, such as impaired sociability. Huh’s and Choi’s labs have traced the effect to elevated maternal levels of a type of immune-signaling molecule called IL-17a, which acts on receptors in brain cells of the developing fetus, leading to hyperactivity in a region of the brain’s cortex called S1DZ. In another study, they’ve shown how maternal infection appears to prime offspring to produce more IL-17a during infection later in life.
Building on these studies, a 2020 paper clarified the fever effect in the setting of autism. This research showed that mice that developed autism symptoms as a result of maternal infection while in utero would exhibit improvements in their sociability when they had infections — a finding that mirrored observations in people. The scientists discovered that this effect depended on over-expression of IL-17a, which in this context appeared to calm affected brain circuits. When the scientists administered IL-17a directly to the brains of mice with autism-like symptoms whose mothers had not been infected during pregnancy, the treatment still produced improvements in symptoms.
New studies and samples
This work suggested that mimicking the “fever effect” by giving extra IL-17a could produce similar therapeutic effects for multiple autism-spectrum disorders, with different underlying causes. But the research also left wide-open questions that must be answered before any clinically viable therapy could be developed. How exactly does IL-17a lead to symptom relief and behavior change in the mice? Does the fever effect work in the same way in people?
In the new project, Choi and Huh hope to answer those questions in detail.
“By learning the science behind the fever effect and knowing the mechanism behind the improvement in symptoms, we can have enough knowledge to be able to mimic it, even in individuals who don’t naturally experience the fever effect,” Choi says.
Choi and Huh will continue their work in mice seeking to uncover the sequence of molecular, cellular and neural circuit effects triggered by IL-17a and similar molecules that lead to improved sociability and reduction in repetitive behaviors. They will also dig deeper into why immune cells in mice exposed to maternal infection become primed to produce IL-17a.
To study the fever effect in people, Choi and Huh plan to establish a “biobank” of samples from volunteers with autism who do or don’t experience symptoms associated with fever, as well as comparable volunteers without autism. The scientists will measure, catalog, and compare these immune system molecules and cellular responses in blood plasma and stool to determine the biological and clinical markers of the fever effect.
If the research reveals distinct cellular and molecular features of the immune response among people who experience improvements with fever, the researchers could be able to harness these insights into a therapy that mimics the benefits of fever without inducing actual fever. Detailing how the immune response acts in the brain would inform how the therapy should be crafted to produce similar effects.
"We are enormously grateful and excited to have this opportunity," Huh says. "We hope our work will ‘kick up some dust’ and make the first step toward discovering the underlying causes of fever responses. Perhaps, one day in the future, novel therapies inspired by our work will help transform the lives of many families and their children with ASD [autism spectrum disorder]."