Amblyopia is the most common cause of vision loss in children, according to the U.S. National Eye Institute. It arises when visual experience is disrupted during infancy, for example by a cataract in one eye. Even after the cataract is removed, vision through the affected eye is impaired because of a failure of this eye to develop strong connections in the brain. The current treatment of covering the “good” eye with a patch to strengthen the amblyopic one is only partially effective and cannot help after a “critical period” ends before age 8.
In a new study, MIT and Dalhousie University neuroscientists demonstrate that by temporarily anesthetizing the retina of the good eye, they could lastingly improve vision in the amblyopic one, even after the critical period in two different mammal species.
The encouraging results support further preclinical testing of the novel therapy, in which the non-amblyopic eye’s retina is temporarily and reversibly silenced by an injection of tetrodotoxin (TTX), says Mark Bear, Picower Professor of Neuroscience in The Picower Institute for Learning and Memory at MIT and corresponding author of the study published in eLife.
“We observed a recovery in every animal,” says Bear, a faculty member of MIT’s Department of Brain and Cognitive Sciences. “We’ve done much better than anyone would have anticipated.”
The results provide hope that the approach can eventually be translated to people, adds Kevin Duffy, professor in the Department of Psychology and Neuroscience at Dalhousie.
“These are remarkable data that demonstrate an unequaled profile of recovery,” says Duffy, who co-led the study with Ming-fai Fong, a postdoc in Bear’s Picower Institute lab. “I am hopeful and optimistic that this study can provide a pathway for a new and more effective approach to amblyopia treatment. I am very proud to have been part of this rewarding collaboration.”
A new approach to amblyopia
The new approach is based on decades of underlying neuroscience discoveries led by Bear that have revealed how amblyopia develops. When input from an amblyopic eye is weak, key connections, or “synapses,” in neural circuits leading from the eye to the brain’s visual cortex wither via a process he discovered called “long-term depression.” But theoretical and experimental studies by his lab have also shown that completely but temporarily suspending visual input creates a condition in which the synaptic connections can fully restrengthen, almost as if they are being “rebooted.”
In 2016, Bear, Duffy, Fong, and colleagues showed they could restore vision in amblyopic mice past the critical period by temporarily inactivating both retinas with TTX, but in the new study they sought to determine whether vision could recover by temporarily suspending retinal activity in just the non-amblyopic eye in older animals, Fong says.
“These differences may seem small, but they are a big deal for a couple of reasons,” she says. “First, inactivating both retinas effectively eliminates vision; even if temporary, this presents some practical challenges. Therefore, our ability to limit inactivation just to one eye makes it potentially more tractable for clinical translation. Second, there is currently no treatment for adult amblyopia in humans. In our study we used mature amblyopic animals that are recalcitrant to any other treatment due to the decline in the capacity for plasticity that comes with age.”
The authors also sought to confirm their result in more than one species to ensure the effect generalizes to the mammalian brain. There is good reason to think so. Clinical observations in humans show that in some cases when a person with amblyopia loses their non-amblyopic eye to disease or injury, their amblyopic eye can improve even if they are adults.
In the new study the team therefore tested whether administering TTX in the non-amblyopic eye of animal models would produce a full recovery of visual response in their amblyopic eye beyond the critical period. Not only did it do so in each animal tested, but also, visual responses always recovered to normal levels in the eye that received the TTX.
“This is a very clear demonstration of how understanding principles of synaptic plasticity can yield a novel therapeutic strategy,” Bear says.
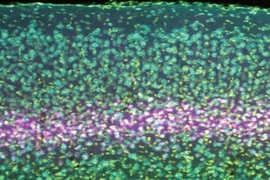
The researchers even showed that neurons that relay visual input to the visual cortex that shrink with amblyopia were able to regain normal size.
The effect of the therapy was stronger and more consistent than in the human clinical cases of non-amblyopic eye loss because once synaptic connections are rebooted for the amblyopic eye and retinal activity returns in the non-amblyopic eye, they become mutually reinforcing, Bear says.
The results lend support for the theory that temporary inactivation of the non-amblyopic eye sets the stage for permanent strengthening of the synapses from the amblyopic eye. This theory holds that when activity is completely absent from the non-amblyopic eye, the degree of input through the amblyopic eye becomes sufficient to trigger synaptic strengthening, or “long-term potentiation.”
Next steps
Theory, however, doesn’t need to be resolved for the promising results to take next steps toward clinical use, the authors note. Instead, Bear says he plans to pursue new studies to ensure that the approach would be safe and effective for people such as adults for whom patch therapy is no longer plausible.
In addition to Fong, Duffy, and Bear, the paper’s other authors are Madison Leet and Christian Candler of The Picower Institute.
The U.S. National Eye Institute, the Canadian Institutes of Health Research, and the JPB Foundation provided support for the research.