One promising strategy to treat cancer is stimulating the body’s own immune system to attack tumors. However, tumors are very good at suppressing the immune system, so these types of treatments don’t work for all patients.
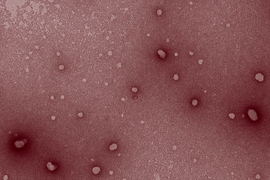
MIT engineers have now come up with a way to boost the effectiveness of one type of cancer immunotherapy. They showed that if they treated mice with existing drugs called checkpoint inhibitors, along with new nanoparticles that further stimulate the immune system, the therapy became more powerful than checkpoint inhibitors given alone. This approach could allow cancer immunotherapy to benefit a greater percentage of patients, the researchers say.
“These therapies work really well in a small portion of patients, and in other patients they don’t work at all. It’s not entirely understood at this point why that discrepancy exists,” says Colin Buss PhD ’20, the lead author of the new study.
The MIT team devised a way to package and deliver small pieces of DNA that crank up the immune response to tumors, creating a synergistic effect that makes the checkpoint inhibitors more effective. In studies in mice, they showed that the dual treatment halted tumor growth, and in some cases, also stopped the growth of tumors elsewhere in the body.
Sangeeta Bhatia, the John and Dorothy Wilson Professor of Health Sciences and Technology and Electrical Engineering and Computer Science, and a member of MIT’s Koch Institute for Integrative Cancer Research and the Institute for Medical Engineering and Science, is the senior author of the paper, which appears this week in the Proceedings of the National Academy of Sciences.
Removing the brakes
The human immune system is tuned to recognize and destroy abnormal cells such as cancer cells. However, many tumors secrete molecules that suppress the immune system in the environment surrounding the tumor, rendering the T cell attack useless.
The idea behind checkpoint inhibitors is that they can remove this “brake” on the immune system and restore T cells’ ability to attack tumors. Several of these inhibitors, which target checkpoint proteins such as CTLA-4, PD-1, and PD-L1, have been approved to treat a variety of cancers. These drugs work by turning off checkpoint proteins that prevent T cells from being activated.
“They work incredibly well in some patients, and they’ve given what some would call cures, for about 15 to 20 percent of patients with particular cancers,” Bhatia says. “However, there’s still a lot more to do to open up the possibility of using this approach for more patients.”
Some studies have found that combining checkpoint inhibitors with radiation therapy can make them more effective. Another approach that researchers have tried is combining them with immunostimulatory drugs. One such class of drugs is oligonucleotides — specific sequences of DNA or RNA that the immune system recognizes as foreign.
However, clinical trials of these immunostimulatory drugs have not been successful, and one possible reason is that the drugs are not reaching their intended targets. The MIT team set out to find a way to achieve more targeted delivery of these immunostimulatory drugs, allowing them to accumulate at tumor sites.
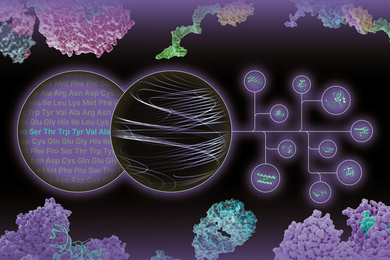
To do that, they packaged oligonucleotides into tumor-penetrating peptides that they had previously developed for delivering RNA to silence cancerous genes. These peptides can interact with proteins found on the surfaces of cancer cells, helping them to specifically target tumors. The peptides also include positively charged segments that help them penetrate cell membranes once they reach the tumor.
The oligonucleotides that Bhatia and Buss decided to use for this study contain a specific DNA sequence that often occurs in bacteria but not in human cells, so that the human immune system can recognize it and respond. These oligonucleotides specifically activate immune cell receptors called toll-like receptors, which detect microbial invaders.
“These receptors evolved to allow cells to recognize the presence of pathogens like bacteria,” Buss says. “That tells the immune system that there’s something dangerous here: Turn on and kill it.”
A synergistic effect
After creating their nanoparticles, the researchers tested them in several different mouse models of cancer. They tested the oligonucleotide nanoparticles on their own, the checkpoint inhibitors on their own, and the two treatments together. The two treatments together produced the best results, by far.
“When we combined the particles with the checkpoint inhibitor antibody, we saw a vastly improved response relative to either the particles alone or the checkpoint inhibitor alone,” Buss says. “When we treat these mice with particles and the checkpoint inhibitor, we can stop their cancer from progressing.”
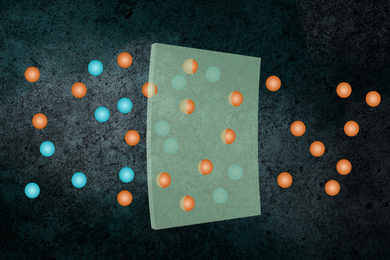
The researchers also wondered whether they could stimulate the immune system to target tumors that had already spread through the body. To explore that possibility, they implanted mice with two tumors, one on each side of the body. They gave the mice the checkpoint inhibitor treatment throughout the entire body but injected the nanoparticles into only one tumor. They found that once T cells had been activated by the treatment combination, they could also attack the second tumor.
“We saw some signs that you could stimulate in one location and then get a systemic response, which was encouraging,” Bhatia says.
The researchers now plan to perform safety testing of the particles, in hopes of further developing them to treat patients whose tumors don’t respond to checkpoint inhibitor drugs on their own. To that end, they are working with Errki Ruoslahti of the Sanford Burnham Prebys Medical Discovery Institute, who originally discovered the tumor-penetrating peptides. A company that Ruoslahti founded has already taken other versions of the tumor-penetrating peptides into human clinical trials to treat pancreatic cancer.
“That makes us optimistic about the potential to scale up, manufacture them, and advance them to help patients,” Bhatia says.
The research was funded by the Koch Institute Support (core) Grant from the National Cancer Institute, a Core Center Grant from the National Institute of Environmental Health Sciences, and the Koch Institute’s Marble Center for Cancer Nanomedicine. Bhatia also has affiliations with the Ludwig Institute for Cancer Research, the Broad Institute of MIT and Harvard, the Wyss Institute for Biologically Inspired Engineering, the Howard Hughes Medical Institute, and Brigham and Women’s Hospital.