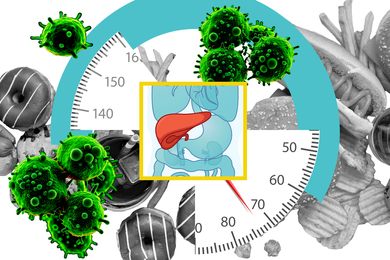
The symptoms of angina — the pain that occurs in coronary artery disease — do not differ substantially between men and women, according to the results of an unusual new clinical trial led by MIT researchers.
The findings could help overturn the prevailing notion that men and women experience angina differently, with men experiencing “typical angina” — pain-type sensations in the chest, for instance — and women experiencing “atypical angina” symptoms such as shortness of breath and pain-type sensations in the non-chest areas such as the arms, back, and shoulders. Instead, it appears that men and women’s symptoms are largely the same, say Karthik Dinakar, a research scientist at the MIT Media Lab, and Catherine Kreatsoulas of the Harvard T.H. Chan School of Public Health.
Dinakar and his colleagues presented the results of their HERMES angina trial at the European Society of Cardiology’s annual congress in September. Their research is one of the first clinical trials accepted at the prestigious conference to use machine learning techniques, which were used to characterize the full range of symptoms experienced by individual patients and to capture nuances in how they described their symptoms in a natural language exchange.
The trial included 637 patients in the United States and Canada who had been referred for their first coronary angiogram, the gold-standard test to diagnose coronary artery disease. After analyzing the language expressed in recorded conversations between physicians and patients and in interviews with patients, the researchers found that almost 90 percent of women and men reported chest pain as a symptom.
Women reported significantly more angina symptoms than men, but the machine learning algorithms identified nine clusters of symptoms, such as “chest sensations and physical limitations” and “non-chest area and associated symptoms” where there were no significant differences among men and women with blockages in their heart.
“This work, showing no real differences between women and men in chest pain, goes against the dogma and will shake up the field of cardiology,” says Deepak L. Bhatt, executive director of Interventional Cardiovascular Programs at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, a co-author of the study. “It is also exciting to see an application of machine learning in health care that actually worked and isn’t just hype,” he adds.
“This sophisticated machine learning study suggests, alongside several other recent more conventional studies, that there may be fewer if any differences in symptomatic presentation of heart attacks in women compared to men,” says Philippe Gabriel Steg, a professor of cardiology at Université Paris- Diderot and director of the Coronary Care Unit of Hôpital Bichat in Paris, France.
“This has important consequences in the organization of care for patients with suspected heart attacks, in whom diagnostic strategies probably need to be similar in women and men,” adds Steg, who was not involved with the MIT study.
Lensing offers a new look
The idea of applying machine learning to cardiology came when Catherine Kreatsoulas, then a Fulbright fellow and heart and stroke research fellow at the Harvard School of Public Health, met Dinakar after a talk in 2014 by noted linguist Noam Chomsky. An interest in language drew them both to the talk, and Kreatsoulas in particular was concerned about the differences in the way men and women express their symptoms, and how physicians might be understanding — or misunderstanding — the way men and women speak about their heart attack symptoms.
In the United States and Canada, 90 percent of cardiologists are male, and Kreatsoulas thought, “‘could this be a potential case of ‘lost in translation?’,” she says.
Kreatsoulas also was concerned that doctors might be misdiagnosing or underdiagnosing female patients — as well as men who didn’t express “typical” angina symptoms — “because doctors have this frame, given their years of medical training in cardiology, that men and women have different symptoms,” Dinakar explains.
Dinakar thought a machine learning framework called “lensing” that he had been working on for crisis counseling might offer a new way of understanding angina symptoms. In its simplest form, lensing acknowledges that different participants bring their own viewpoint or biases to a collective problem or conversation. By developing algorithms that include these different lenses, researchers can retrieve a more complete picture of the data provided by real-world conversations.
“When we train machine learning models in situations like the heart disease diagnosis, it is important for us to capture, in some way, the lens of the physician and the lens of the patient,” says Dinakar.
To accomplish this, the researchers audio-recorded two clinical interviews, one of patients describing their angina symptoms in clinical consult interviews with physicians and one of patient-research assistant conversations “to capture in their own natural words their descriptions of symptoms, to see if we could use methods in machine learning to see if there are a lot of differences between women and men,” he says.
In a typical clinical trial, researchers treat “symptoms as check boxes” in their statistical analyses, Dinakar notes. “The result is to isolate one symptom from another, and you don’t capture the entire patient symptomatology presentation — you begin to treat each symptom as if it’s the same across all patients,” says Dinakar.
“Further, when analyzing symptoms as check boxes, you rarely see the complete picture of the constellation of symptoms that patients actually report. Often this important fact is compensated for poorly in traditional statistical analysis,” Kreatsoulas says.
Instead, the lensing model allowed the scientists “to represent each patient as a unique fingerprint of their symptoms, based on their natural language,” says Dinakar.
Seeing patients in this way helped to uncover clusters of symptoms that could be compared in men and women, leading to the conclusion that there were few differences in symptoms between these two groups of patients.
"The terms ‘typical’ and ‘atypical’ angina should be abandoned, as they do not correlate with disease and may perpetuate stereotypes based on sex," Dinakar and his colleagues conclude.
Helping doctors think deeper
The goal of clinical trials like the HERMES trial is not to “replace cardiologists with an algorithm,” says Dinakar. “It’s just a more sophisticated way of doing statistics and bringing them to bear on an urgent problem like this.”
In the medical realm, the unique lens of each patient and physician might typically be thought of as “bias” in the pejorative sense — data that should be ignored or tossed out of an analysis. But the lensing algorithms treat these biases as information that can provide a more complete picture of a problem or reveal a new way of considering a problem.
In this case, Dinakar said, “bias is information, and it helps us to think deeper. It’s very important that we capture that and try to represent that the best we can.”
Although machine learning in medicine is often seen as a way to “brute force” through problems, like identifying tumors by applying image recognition software and predictive algorithms, Dinakar hopes that models like lensing will help physicians break down “ossified” frames of thinking across medical challenges.
Dinakar and Kreatsoulas are now applying the machine learning models in a clinical trial with neuro-gastroenterology researchers at Massachusetts General Hospital to compare physician lenses in diagnosing diseases such as functional gastrointestinal disease and irritable bowel syndrome.
“Anything we can do in statistics or machine learning in medicine to help break down an ossified frame or broken logic and help both providers and patients think deeper in my opinion is a win,” he says.