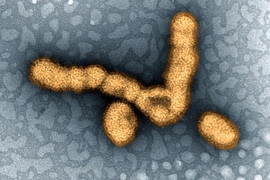
How can we better avoid the flu? A new paper co-authored by researchers at MIT examines the best ways to reduce the likelihood that individuals and groups will become infected with the flu, both by diligent use of non-pharmeceutical interventions (NPIs) and by effective deployments of vaccine.
The paper, "Engineering Effective Responses to Influenza Outbreaks," has been published in Service Science by Stan N. Finkelstein, senior research scientist in MIT's Engineering Systems Division and the Harvard-MIT Division of Health Sciences and Technology and associate professor of medicine at Harvard Medical School; Richard C. Larson, the Mitsui Professor of Engineering Systems at MIT and principal investigator of the MIT BLOSSOMS Initiative; Karima Nigmatulina PhD '09, general director at the Institute of Master Planning for the city of Moscow in Russia; Anna Teytelman '08 PhD '12, a software engineer at Google.
The researchers argue that the mean number of new flu infections directly generated by a 'typical' newly infected person in a fully susceptible population — known as R0 — is local and contextual and can be moved up or down in numerical value by actions of individuals in the local environment. The paper’s mathematical models and analysis of historical events, plus conversations with flu experts, suggest that R0 does not exist as a single value, and it should not be announced, such as by the World Health Organization or the U.S. Centers for Disease Control and Prevention (CDC), in that way.
The second key finding relates to deployment of flu vaccines when they arrive late and in small quantities when confronting a novel flu virus, as with H1N1 in 2009. The current CDC vaccine deployment plan distributes vaccine units to states in direct proportion to the U.S. Census population of each state, regardless of progression of the flu wave in each state. Such a plan can deliver vaccines to states whose flu waves have already come and gone, meaning that the vaccines in those states will be of no value. And those misdirected vaccine units could prove quite beneficial in averting flu infections in other states whose flu waves have not yet peaked. The paper projects that up to 5 million Americans who became ill with H1N1 flu in 2009 might not have become infected if an alternative, more adaptive vaccine allocation plan had been in effect. The paper provides the essentials for such a new plan.
This research has been sponsored by IBM, the Sloan Foundation of New York, and the CDC via a collaboration with the Harvard T.H. Chan School of Public Health Center for Public Health Preparedness.