CAMBRIDGE, Mass. -- A researcher at the Massachusetts Institute of Technology has developed "decoy" compounds that can render harmless the toxic fibrils that grow in the brains of Alzheimer's patients.
Published recently in the Journal of Alzheimer's Disease, the work by biologist Vernon M. Ingram, John and Dorothy Wilson Professor at MIT, presents another potential point of attack against Alzheimer's disease.
The discovery may lead to "a suitable therapeutic strategy early in the course of the disease, when the beta-amyloid fibrils begin to form," Ingram said.
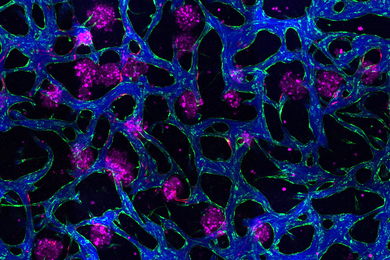
In patients with Alzheimer's disease, a common protein gone haywire produces an abnormal amount of beta-amyloid peptides in the brain. These aggregate into fibrils, or plaques, that cause a deadly influx of calcium into neurons when they come in contact with them.
Ingram and a research team comprised of his long-time colleague, MIT technical associate Barbara Blanchard, and a group of MIT undergraduates created decoy peptides that combine with the amyloid peptide and prevent its calcium-raising toxicity.
INSIDIOUS RIBBONS
In Alzheimer's patients, plaques develop early in areas of the brain used for memory and other cognitive functions. The loss of memory and thinking ability characteristic of the disease are related to the dysfunction and eventual death of certain brain cells.
Fibrils of amyloid peptide molecules stack together to form a long, ribbon-like peptide arrays that aggregate to form the characteristic Alzheimer plaques. The plaques consist of insoluble deposits of beta-amyloid, a protein fragment snipped from a larger protein called amyloid precursor protein (APP). The formation of these pathological peptides is partially understood. It appears that only the aggregated fibrillar forms of the beta-amyloid peptide are toxic.
When these fibrils contact neurons, they open channels in the cell that allow large amounts of calcium to enter. Elderly brain cells are particularly vulnerable to this because they have diminished ability to use the tactics cells normally use to get rid of excess calcium.
Calcium helps cells do many things, including carry nerve signals. Neurons normally are very careful about the amount of calcium they allow in because they use minute changes in levels of internal calcium to interpret messages from other neurons. Too much calcium inside cells leads to cell death.
IDEAL DRUG CANDIDATES
Researchers are approaching the battle against Alzheimer's with a number of strategies. "Our approach is to try to find small peptides that will prevent the amyloid peptide from being toxic and render it harmless," Ingram said.
To do this, the researchers selected from a combinatorial library a series of peptides with various interesting properties. Peptides are natural or synthetic compounds of two or more linked amino acids, the most basic building blocks of life.
Ingram and his research team created 30 small peptides, each between five and eight amino acids long, and tested them with lab-cultured human nerve cells. Some had no effect. Eight of them counteracted the excessive, toxic influx of calcium, knocking it down to normal levels. "In the presence of the decoy peptide, the final product of the aggregate is not toxic," Ingram said. The fibrils still form, but are harmless and do not effect internal calcium levels in the cells.
Because they are small and can be modified to cross the blood-brain barrier, "our decoy peptides are obvious candidates for drug development," Ingram said.
Peptides are ideal drug candidates because they are highly specific -- they work only with certain substances, like keys that fit only one lock. The peptides Ingram studies also are resistant to degradation, meaning that they may survive a trip through the body's digestive system and make their way to their target in the brain.
"Experience with a number of difficult diseases teaches us that more than a single therapeutic strategy is often needed, because the dosage might be so high to cause unacceptable side effects," he said.
These decoy peptides also may be effective in the treatment of another neurodegenerative condition -- Huntington's disease. The mutant Huntington protein forms aggregates by a related process inside individual neurons. Ingram plans to test the decoy method as a way to intercept the toxic aggregates of mutant proteins responsible for Huntington's disease.
This work is supported by Amgen Inc., the Kurt & Johanna Immerwahr Fund for Alzheimer's Research and MIT's Undergraduate Research Opportunities Program.