Surgeons around the country are now being trained in implanting artificial skin on burn patients, culminating years of work by Ioannis V. Yannas, professor of polymer science and engineering, who is continuing research into applying his methods to replacing other damaged body parts.
Patients with severe burns have lost their dermis, a layer about two millimeters thick that lies beneath the epidermis and which does not regenerate when damaged. Traditionally, such patients receive autografts, or skin transplants from donor sites elsewhere on their bodies. But this method has its drawbacks. The donor graft is usually smaller than the wound being repaired; slits are cut in the skin graft so it can be stretched, and scarring occurs at each slit. There is also some scarring at the donor site, where about half the thickness of the dermis has been removed.
The technology developed by Professor Yannas and his colleagues (which received FDA approval in early March) involves chemically bonding collagen taken from animal tendons with glycosaminoglycan (GAG) molecules from animal cartilage to create a simple model of the extracellular matrix that provides the basis for a new dermis. Collagen is part of the structural scaffolding in mammals (analogous to cellulose in plants) that allows tissues to maintain their shape. The collagen-GAG combination "makes a simple chemical analog of the matrices in our own tissues," he explained.
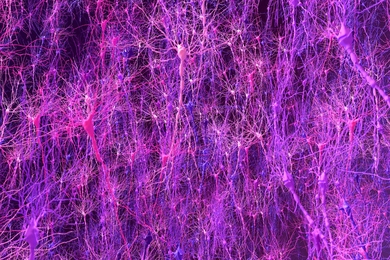
Surgeons can implant this material, temporarily covered by a thin layer of silicone that protects the area from infectious agents and excessive moisture loss. The collagen-GAG material has pores with carefully controlled diameters that permit cells to grow through the scaffold, which is eventually broken down and dissolved by enzymes. Cells synthesize a new dermis at the same time that the scaffold is being broken down. Epidermis then grows naturally over the new dermis unless the wound area is especially large, in which case the surgeon does an autograft of epidermis-a much less problematic procedure than grafting dermis, because epidermis is one-tenth as thick and is constantly being shed and regrown.
Patients end up almost completely free of the devastating scars that result from ungrafted burns (scar tissue is weaker and less flexible than skin) or the somewhat lesser but still significant disfigurement from autografts. The new skin also grows as the patients do, an important consideration for burned children.
The only limitation is that patients with large grafts must avoid strenuous exercise in the sun, because the newly synthesized dermis does not have the original dermis's sweat glands and hair follicles. But the technique goes a long way toward solving "the short-term problem of survival and the long-term problem of quality of life," said Professor Yannas, who holds appointments in the Departments of Mechanical Engineering and Materials Science and Engineering. He is a consultant for Integra LifeSciences Corp., the New Jersey firm that licensed his technology from MIT.
In addition to several students, Professor Yannas' collaborator has been Dr. John F. Burke, professor emeritus of surgery at Harvard Medical School and Massachusetts General Hospital. Dr. Burke pioneered development of the procedure for preparing wounds for collagen-GAG grafts by removing all traces of dead tissue. He also educated the MIT team as to the specific requirements of wound treatment for massively burned patients, as well as being the first surgeon to use the new treatment with humans. Professor Yannas's work has focused on optimizing the pore size and rate of breakdown of the material, as well as its chemical composition. He has found that the structural requirements are critical enough to define a biologically active, insoluble macromolecular network, the first of its kind.
Professor Yannas and graduate students Albert Chang and Lila Chamberlain have also had significant success with animals in using a different collagen-GAG matrix to bridge severed nerve segments in limbs. A degradable tube filled with the different matrix analog is attached to each severed end, and nerve axons grow into the matrix, making a functional connection between the cut ends. Nerve autografts have been used in human patients but with only limited success; the affected limb regains some control but is far short of having normal coordination. Another team at San Francisco Presbyterian Hospital has licensed the MIT technology to regenerate the knee meniscus, the tissue that is often torn in injuries. Though current surgical techniques can trim off jagged edges that cause pain, the meniscal tissue can't be replaced after it's removed or wears down.
"What we're finding is that regeneration is an approach that can be used for different organs," Professor Yannas said. The work may eventually lead to improved methods for repairing body parts that are now replaced with wholly synthetic biomechanical devices (for example, artificial hips and heart valves made of metals, plastics and ceramics) or organs harvested from other people (transplanted hearts, kidneys, etc.). Artificial parts are typically incompatible with adjacent tissues and eventually fail or cause problems for the host, while transplants are hampered by rejection by the immune system and a shortage of donors.
The advances are especially exciting because they appear to involve a repetition of the process that took place even before birth. "Information that a fetus uses to build skin is probably being used for the second time," he said. "Adult mammals don't normally resynthesize organs they've lost, but now they're doing it."
The research was supported by NSF and NIH grants.