Experiments by three MIT scientists published in the August 11 issue of Science have shown that drugs such as insulin can theoretically be administered to patients through a skin patch with the aid of ultrasound, rather than orally or by injection.
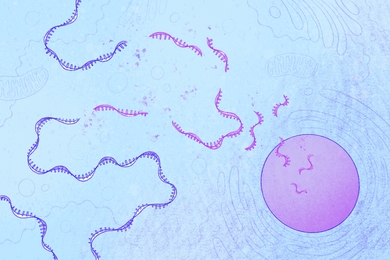
A few drugs are already taken by some people via transdermal patches. However, this method of drug administration is effective only with substances having a low molecular weight; skin has extremely low permeability, so large molecules cannot readily pass through. The low permeability is a result of the structure of the outermost skin layer, which consists of flat dead cells filled with keratin fibers surrounded by fatty layers.
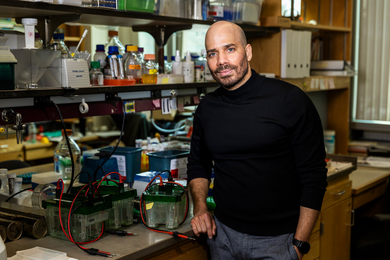
Professors Daniel Blankschtein and Robert Langer and graduate student Samir Mitragotri of the Department of Chemical Engineering used applications of low-frequency ultrasound to significantly increase skin permeability, allowing effective transmission of insulin, a large protein that is used to treat diabetes.
Other drugs in this category that were administered in this way in the experiments include gamma-interferon (used to boost the immune systems in patients suffering from viral infection or cancer) and erythropoeitin (used to treat severe anemia). These substances are roughly 100 times the molecular weight of drugs now administered through skin patches, such as estradiol for estrogen replacement in post-menopausal women, nicotine for smoking cessation, and nitroglycerine for alleviating angina.
Work done in 1989 by Dr. Langer and Joseph Kost (a former MIT postdoctoral fellow) showed that ultrasound could be used to enhance transport of drugs (though not specifically proteins) through the skin in a phenomenon known as sonophoresis. This method is superior to conventional means of administration because it provides sustained release of the drug for up to seven days, and it is easier than injection and eliminates the risk of infection. Also, when proteins are administered orally, they are susceptible to gastrointestinal degradation and are not taken up by the bloodstream efficiently.
Recent work by the three authors and David Edwards (another former postdoctoral fellow with Dr. Langer) showed that application of ultrasound at a frequency of 1 MHz aided transport through the skin of low-molecular-weight drugs by causing cavitation, or growth and oscillation of the air pockets in the keratin fibers of skin. The oscillations disorganize the intervening fatty layers, which eases the flow of molecules through the skin. Drs. Langer and Blankschtein and Mr. Mitragotri theorized that a lower frequency of ultrasound waves would make transdermal transport even easier, since it is known that cavitational effects increase as frequency is lowered.
Results showed that human cadaver skin was made significantly more permeable with the application of ultrasound frequencies of 20 KHz (which is a much lower frequency than the ultrasound now used to visualize babies). Experiments on hairless rats also revealed that insulin could be effectively administered in this way, as measured both by the level of insulin detected in the blood and by the resulting drop in blood glucose levels.
The experiments further demonstrated that ultrasound does not result in any permanent damage to the skin's barrier properties or to the underlying muscle tissues. Low-frequency ultrasound is already used by dentists for tooth-cleaning, but the scientists emphasized that more research is needed on sonophoresis's effects on the body and the immune system (as well as on optimization of frequency, pulse length and intensity) before the technique is ready for everyday use. If it does prove to be safe and effective for people, diabetics could one day wear small devices that would both monitor blood levels and deliver ultrasound through an insulin patch whenever required, eliminating any need for the patient to track and treat his condition.
Ashish Patel, a senior in chemical engineering, and Stanley Liauw, a junior in chemistry, assisted in the research with the support of UROP. Major funders for the work were the National Institutes of Health, Zachary Miller and the Schering Plough Foundation.
A version of this article appeared in MIT Tech Talk on August 16, 1995.